Change Healthcare Notice
In February, our practice was impacted by the national outage experienced by Change Healthcare because of a cyberattack. Change Healthcare is a healthcare technology company, part of Optum and United Healthcare, that provides services used by much of the US healthcare system, including our practice.
We have remained in close contact with Change Healthcare as they investigate and address this issue.
Change Healthcare has begun issuing customer notifications related to the February 2024 cyberattack. On April 22, 2024, Change Healthcare publicly confirmed the impacted data could cover a substantial proportion of people in America. More recently, on June 20, 2024, Change Healthcare notified our practice’s management company that some of its data was compromised.
At this time, Florida Cancer Affiliates has not been notified of any specific patients of the practice whose protected health information has been affected by the incident.
For more information, please visit https://www.changehealthcare.com/hipaa-substitute-notice.
Request a Prescription Refill from Florida Cancer Affiliates
If you are looking to refill a medication dispensed by Florida Cancer Affiliates in Ocala, please fill out the form below. If you have questions about your prescription refill, call us at (352)547-1915.
For all other prescriptions not filled by us, please contact your pharmacy directly.
Coronavirus Advisory
The health and safety of our patients is our top priority. We are closely monitoring COVID-19, including the latest updates from the Centers for Disease Control and Prevention (CDC). The CDC-recommended protocols for healthcare providers regarding COVID-19 are aligned with our existing protocols for flu season. During flu season, we emphasize an array of preventative measures that protect our patients and staff from exposure to illness.
In addition to our existing protocols and our rigorous cleaning procedures, to further ensure the safety of those we serve, we have:
- Implemented travel restrictions for our employees
- Mandated that any employees feeling unwell stay home
- Limited the number of caregivers accompanying patients to only one per visit
- Asked all patients experiencing symptoms of a cough, fever or difficulty breathing; those who traveled to areas impacted by the COVID-19 within the past 14 days or who may have been exposed to the coronavirus to contact Florida Cancer Affiliates before visiting our clinics for scheduled appointments
Pharmacy
Have many of your prescriptions filled at our in-house pharmacy!
-
Prior authorization, grant, and copay assistance experts.
-
Working hand-in-hand with your physicians and prescribers.
-
Prescription refill reminders and ready reminders.
-
Accepting many forms of payment and most insurances.
-
Open Monday to Friday, 8:30am to 5pm, or 24 hours via call center.
Refill prescriptions from Florida Cancer Affiliates here.
For more information, call (352)547-1915 or email us at FCAPharmacy@usoncology.com, or visit us in person at 3130 SW 32nd Ave, Ocala, FL 34474.
See our Medication Refill Policy.
Florida Cancer Affiliates - Ocala is ACHC Accredited
 Ocala, Fl, Florida Cancer Affiliates proudly announces it has achieved accreditation through the Accreditation Commission for Health Care (ACHC) for the services of Specialty Pharmacy.
Ocala, Fl, Florida Cancer Affiliates proudly announces it has achieved accreditation through the Accreditation Commission for Health Care (ACHC) for the services of Specialty Pharmacy.
Accreditation is a process through which healthcare organizations demonstrate compliance with national standards. Accreditation by ACHC reflects an organization’s dedication and commitment to meeting standards that facilitate a higher level of performance and patient care.
ACHC is a nonprofit organization that has stood as a symbol of quality and excellence since 1986. ACHC is ISO 9001:2015 certified and has CMS deeming authority for Home Health, Hospice, and DMEPOS.
Florida Cancer Affiliates is committed to providing patients with the specialized care they need, along with the tools, resources, and personal support that will help them navigate through their journey with cancer. We offer our patients the latest technology and therapies, ranging from leading-edge diagnostic imaging to sophisticated forms of radiation therapy. At the same time, we are dedicated to delivering your care with the compassion you desire. Our patients have access to the best therapies and current treatment options, including clinical trials, right here in our own community.
This specialty accreditation means that Florida Cancer Affiliates can bring more specialized pharmaceutical care to patients without having to rely on outside pharmacies to deliver their oral medications.
Make the best choice for your cancer care. Call for an appointment today.
For more information, call (352)547-1915.
Dr. Nanfro's Retirement & Current Patient Information
If you are a former patient of Dr. John Nanfro’s and you had a future appointment with him, that appointment is cancelled and you must reschedule your appointment.
Florida Cancer Affiliates will continue to provide excellent care for your hematology and oncology needs if you so choose. Patients have the opportunity to reschedule their appointments with physicians in our group, with no records transfer and no headaches. All your information is already in our shared database
The doctors below are listed in order of availability. Please click on the doctor’s name to see physician bio. Our staff will be ready to assist you in transferring your care.
|
850-769-2996 |
850-769-2996 |
850-763-0036 |
850-215-5300 |
850-763-0036 |
|
2614 Jenks Avenue |
2614 Jenks Avenue |
2100 State Avenue |
2417 Jenks Avenue |
2100 State Avenue |
You may also want to contact your referring provider for their preference. Medical records will continue to be held by Florida Cancer Affiliates, and available upon request as always.
Retirement letter from Dr. Nanfro:
Dear Patient
It has been a pleasure to treat patients with cancer and blood disorders for the past 34 years. I have had the privilege serving members of our beautiful community for over 10 years, and have developed lifelong friendships with many of my patients. It’s been an honor to be entrusted with your care.
After lots of soul searching and consulting with my family and friends, I have made a decision to announce my retirement from hematology oncology, effective February 29th, 2016. Over the past three decades, I have cherished the memories I shared with my patients. Working with cancer patients has been a gratifying and rewarding experience for me. I wouldn’t trade that time for anything. I hope you will accept my retirement for what it is: a cherished reward for a lifetime of hard work. I’m ready and excited to begin the next phase in my life.
As I go towards my new adventure, Florida Cancer Affiliates will continue to provide excellent care for your hematology and oncology needs. Patients will have the opportunity to reschedule their appointments with physicians in our group. The doctors above are listed in order of availability. Our staff will ready to assist you in transferring your care. You may also want to contact your referring provider for their preference. I have made arrangements to be available to my partners during this transition phase, and you can be confident you will continue to receive the compassionate and innovative care you’re accustomed to. I have utmost confidence and respect for the doctors in my group. You will be in great hands.
Medical records will continue to be held by Florida Cancer Affiliates, and available upon request as always.
Thank you again for allowing me to serve you as your physician. It has been an honor.
Most sincerely,
John Nanfro, M.D., F.A.C.P.
Payment Success
Thank you for submitting your electronic payment.
For questions or comments please contact: .(JavaScript must be enabled to view this email address)
You may contact us by calling 1-800-998-3450 and a representative will be happy to help you.
Thank you for choosing Florida Cancer Affiliates.
Make a Payment
There are several convenient options for you to make a payment.
- Make a payment at your next in-office visit.
- Pay online
- Pay by phone: 24 hours per day, 7 days per week: (352) 810-3304
- Mail payment to:
Florida Cancer Affiliates
PO BOX 946205
Atlanta, GA 30394-6205
Call with questions about your bill: (800) 630‑4670; Monday – Friday, 8:30AM – 4:30PM (Eastern)
Clinical Trial Locations
BREAST CANCER - Locally Advanced or Metastatic - First Line
For detailed information about any of the following studies, please contact our Research Department at 352-732-4938.
CLINICAL TRIALS:
Lung Cancer
 A Randomized Phase 3 Study of Sitravatinib in Combination With Nivolumab Versus Docetaxel in Patients With Advanced Non-Squamous Non-Small Cell Lung Cancer With Disease Progression On or After Platinum-Based Chemotherapy and Checkpoint Inhibitor Therapy (SAPPHIRE)
A Randomized Phase 3 Study of Sitravatinib in Combination With Nivolumab Versus Docetaxel in Patients With Advanced Non-Squamous Non-Small Cell Lung Cancer With Disease Progression On or After Platinum-Based Chemotherapy and Checkpoint Inhibitor Therapy (SAPPHIRE)
https://clinicaltrials.gov/ct2/show/NCT03906071
Double Blinded, Placebo-Controlled Phase III Study to Evaluate the Efficacy and Safety of Canakinumab Vs Placebo as Adjuvant Therapy in Adult Subjects with Stages II-IIIA and IIIB (T>5cm N2) Completely Resected (R0) Non-Small Cell Lung Cancer (NSCLC)
https://www.clinicaltrials.gov/ct2/show/NCT03447769#contacts
A Phase 2 Randomized, Multicenter, Double-Blind Study of the Glutaminase Inhibitor Telaglenastat with Pembrolizumab and Chemotherapy Versus Placebo with Pembrolizumab and Chemotherapy in First-Line, Metastatic KEAP1/NRF2-Mutated, Nonsquamous, Non-Small Cell Lung Cancer (NSCLC)
https://clinicaltrials.gov/ct2/show/NCT04265534
Study of JNJ-61186372, a Human Bispecific EGFR and cMet Antibody, in Participants With Advanced Non-Small Cell Lung Cancer - Drugs: JNJ-61186372, Lazertinib, Pemetrexed, Carboplatin, JNJ-61186372 - EGFR and MET
https://clinicaltrials.gov/ct2/show/NCT02609776
Breast
 A Phase III, Multicenter, Randomized, Double-blind, Placebo-controlled Study to Assess the Efficacy and Safety of Alpelisib (BYL719) in Combination With Nab-paclitaxel in Patients With Advanced Triple Negative Breast Cancer With Either Phosphoinositide-3-kinase Catalytic Subunit Alpha (PIK3CA) Mutation or Phosphatase and Tensin Homolog Protein (PTEN) Loss Without PIK3CA Mutation
A Phase III, Multicenter, Randomized, Double-blind, Placebo-controlled Study to Assess the Efficacy and Safety of Alpelisib (BYL719) in Combination With Nab-paclitaxel in Patients With Advanced Triple Negative Breast Cancer With Either Phosphoinositide-3-kinase Catalytic Subunit Alpha (PIK3CA) Mutation or Phosphatase and Tensin Homolog Protein (PTEN) Loss Without PIK3CA Mutation
https://www.clinicaltrials.gov/ct2/show/NCT04251533
Evaluation of Lasofoxifene Versus Fulvestrant in Advanced or Metastatic ER+/HER2− Breast Cancer With an ESR1 Mutation - Drugs: Lasofoxifene, Fulvestrant - ESR1 mutations
https://clinicaltrials.gov/ct2/show/NCT03781063
Evaluation of Lasofoxifene Combined With Abemaciclib in Advanced or Metastatic ER+/HER2− Breast Cancer With an ESR1 Mutation - Drugs: Lasofoxifene and abemaciclib (VERZENIO).- ESR1 mutations
https://clinicaltrials.gov/ct2/show/NCT04432454
Solid Tumors
 Phase I/II Study of the Safety, Pharmacokinetics, and Preliminary Clinical Activity of BT8009 in Patients with Nectin-4 Expressing Advanced Malignancies
Phase I/II Study of the Safety, Pharmacokinetics, and Preliminary Clinical Activity of BT8009 in Patients with Nectin-4 Expressing Advanced Malignancies
https://clinicaltrials.gov/ct2/show/NCT04561362?term=BT8009-100&draw=2&rank=1
Phase 1/1b Study to Evaluate the Safety and Activity of TTX-030 (Anti-CD39) in Combination with Budigalimab (Anti-PD-1) and/or mFOLFOX6 in Subjects with Solid Tumors
https://clinicaltrials.gov/ct2/show/NCT04306900
A First-in-human, Phase 1 Study to Evaluate the Safety of TTX-080, an HLA-G Antagonist, in Subjects with Advanced Solid Tumors
https://clinicaltrials.gov/ct2/show/NCT04485013
A phase 1/2 study of IDE196 in patients with solid tumors harboring GNAQ/11 mutations or PRKC fusions Drugs: IDE196 - GNAQ or GNA11 mutations or PRKC fusions
https://clinicaltrials.gov/ct2/show/NCT03947385
A Phase 1/2 Multiple Expansion Cohort Trial of MRTX849 in Patients with Advanced Solid Tumors with KRAS G12C Mutation - Drugs: MRTX849, Pembrolizumab, Cetuximab, Afatinib - KRAS G12C
https://clinicaltrials.gov/ct2/show/NCT03785249 Mutation
A Phase 2 Study of Seribantumab in Adult Patients with Neuregulin-1 (NRG1) Fusion Positive Locally Advanced or Metastatic Solid Tumors - Drugs: Seribantumab - Neuregulin-1 (NRG1) Fusion
https://www.clinicaltrials.gov/ct2/show/NCT04383210
A Phase I/II Study of MCLA-128, a full length IgG1 Bispecific Antibody Targeting HER2 and HER3, in Patients with Solid Tumors - Drugs: zenocutuzumab (MCLA-128) - Neuregulin-1 (NRG1) Fusion
https://clinicaltrials.gov/ct2/show/NCT02912949
A Phase 1/2 Multicenter Study of the Safety, Pharmacokinetics, and Preliminary Efficacy of APL-101 in Subjects with Non-Small Cell Lung Cancer with c-Met EXON 14 Skip Mutations and c-Met Dysregulation Advanced Solid Tumors - Drugs: APL-101 Oral Capsules - c-Met EXON 14 Skip Mutations c-Met Dysregulation
https://www.clinicaltrials.gov/ct2/show/NCT03175224
A Phase 2 Study of Seribantumab in Adult Patients With NRG1 Gene Fusion Positive Cancer - Drugs: Seribantumab - NRG1 Fusion
https://clinicaltrials.gov/ct2/show/NCT04383210
A Study of Erdafitinib in Participants With Advanced Solid Tumors and Fibroblast Growth Factor Receptor (FGFR) Gene Alterations - FGFR
https://clinicaltrials.gov/ct2/show/NCT04083976
A Study of Repotrectinib (TPX-0005) in Patients With Advanced Solid Tumors Harboring ALK, ROS1, or NTRK1-3 Rearrangements - Drugs: Oral repotrectinib (TPX-0005) - ROS1, or NTRK1-3 Rearrangements
https://clinicaltrials.gov/ct2/show/NCT03093116
B-Cell Lymphoma and Non-Hodgkin's Lymphoma
PK,PD, Safety and Tolerability of Multiple Dose Regimens of MT-3724 With Lenalidomide for the Treatment of Patients With Relapsed/Refractory Diffuse Large B Cell Non-Hodgkin's Lymphoma (MT-3724_NHL_003) - Drugs: MT-3724 - CD20
https://clinicaltrials.gov/ct2/show/NCT03645395
PK,PD, Safety and Tolerability of Multiple Dose Regimens of MT-3724 With Gemcitabine and Oxaliplatin for the Treatment of Patients With Relapsed/Refractory Diffuse Large B Cell Non-Hodgkin's Lymphoma - Drugs: MT-3724 - CD20
https://clinicaltrials.gov/ct2/show/NCT03488251
A Randomized Phase 3 Study to Evaluate the Efficacy and Safety of Enzastaurin Plus R-CHOP Versus R-CHOP in Treatment-Naïve Subjects with High-Risk Diffuse Large B-Cell Lymphoma Who Possess the Novel Genomic Biomarker DGM1™ - Drugs: Enzastaurin (Kinenza®), R-CHOP, Placebo - Positive for Genomic Biomarker DGM1
https://clinicaltrials.gov/ct2/show/NCT03263026
Unresectable or Metastatic Melanoma
Open-label, Active-controlled, Multicenter Phase II Study to Investigate the Efficacy and Safety of UV1 Vaccination in Combination with Nivolumab and Ipilimumab as First-line Treatment of Patients with Unresectable or Metastatic Melanoma (UV1-202)
https://clinicaltrials.gov/ct2/show/NCT04382664
Prostate
A Study of Niraparib in Combination With Abiraterone Acetate and Prednisone Versus Abiraterone Acetate and Prednisone for Treatment of Participants With Metastatic Prostate Cancer - Drugs: Niraparib, Abiraterone Acetate, Prednisone, Placebo - BRCA 1/2 and CDK12
https://clinicaltrials.gov/ct2/show/NCT03748641
Gastric or Gastroesophageal Junction Cancer
A Phase 2/3 Trial to Evaluate Margetuximab in Combination with Chemotherapy and CPI or Trastuzumab and Chemotherapy alone in Patients with Treatment-naïve Metastatic or Locally Advanced, Her2-positive Gastric or Gastroesophageal Junction Cancer
https://clinicaltrials.gov/ct2/show/NCT04082364
Polycythemia Vera
A Phase 2 Study of the Hepcidin Mimetic PTG-300 in Patients with Phlebotomy-Requiring Polycythemia Vera
https://clinicaltrials.gov/ct2/show/NCT04057040
Primary Immune Thrombocytopenia (ITP)
A Phase 3, Multicenter, Randomized, Double-Blinded, Placebo-Controlled Trial to Evaluate the Efficacy and Safety of Efgartigimod (ARGX-113) 10 mg/kg IV in Adult Patients with ITP
https://clinicaltrials.gov/ct2/show/NCT04188379
Folicular Lymphoma
Double-blinded, Placebo-controlled Phase 3 Study of the Bruton’s Tyrosine Kinase (BTK), Ibrutinib, in Combination with Rituximab versus Placebo in Combination with Rituximab in Treatment Naïve Subjects with Follicular Lymphoma
https://clinicaltrials.gov/ct2/show/study/NCT02947347
Supportive Care
A Randomized, Dose-ranging, Open-label, Parallel Group Study to Assess the Efficacy, Safety and Pharmacokinetics of Palonosetron HCl Buccal Film versus IV Palonosetron 0.25 mg (ALOXI®) for the Prevention of Chemotherapy-induced Nausea and Vomiting in Cancer Patients Receiving Moderately Emetogenic Chemotherapy
https://www.clinicaltrials.gov/ct2/show/NCT04592198
Targeted Therapy Trails
We have access to over 30 trials through Tempus’ and Caris PharmaTech’s Just-in-Time activation program. These trials can be activated within 2 weeks of identifying an eligible sub
Clinical Trials & Research
Leading Research. Promising Drug Trials.
Over the past 40 years, Ocala Oncology/Florida Cancer Affiliates has provided our patients access to cutting-edge and innovative clinical trials in a comfortable and convenient setting. One of the largest and most reputable community-based research networks in the world, US Oncology Research has contributed to over 70 FDA-approved cancer therapies and approximately one-third of all FDA-approved oncology therapies. It also specializes in Phase I–IV oncology clinical trials and has participated in over 1,600 investigator-initiated and sponsor-initiated trials since its inception. The program brings innovative therapies and clinical trials to practices and patients in communities across the nation to help advance the science of cancer care while offering the best possible treatments and improved patient outcomes.
We are proud of our new role in the research and development of vital new cancer therapies through independent studies. This will alow us broader range of opportunities to offer our patients . We are dedicated to advancing cancer care by leading and participating in clinical trials that test the safety and efficiency of new or modified treatments. And we are deeply committed to bringing clinical trials to our community, offering patients an opportunity to help shape the future of cancer treatment, while benefitting from the very latest in clinical trials. Ocala Oncology/Florida Cancer Affiliates is constantly offering eligible patients opportunities to join new trials.
At Ocala Oncology/Florida Cancer Affiliates,research is an integral part of our comprehensive efforts to provide cancer patients in our community with access to the latest and most advanced therapies and treatment options. We now have access to Sarah Cannon Research Trials.
We are pleased to share this list of clinical trials currently enrolling at our practice.
MYLUNG Consortium™ research study in metastatic non-small cell lung cancer (mNSCLC)
I am pleased to share an update regarding our progress with the MYLUNG Consortium™ research study in metastatic non-small cell lung cancer (mNSCLC). Results from the first phase were released during the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting by The US Oncology Network (The Network), US Oncology Research and Ontada™.
Makenzi Evangelist, MD, physician lead for the study and oncologist with New York Oncology Hematology, presented the findings during an oral presentation at ASCO titled, “Biomarker tissue journey among patients with untreated metastatic non-small cell lung cancer (mNSCLC) in The US Oncology Network community practices.” (ASCO Abstract 9004)
Protocol 1 (out of 3) provides a retrospective look at chart data and allows us to draw early conclusions about historical baseline trends for testing patterns and identify gaps in the data that need to be filled with the prospective research the MYLUNG Consortium will address in the next protocol.
Protocol 1 findings include:
- Most patients had at least one biomarker test result prior to first-line therapy
- Fewer than 50% of patients had all five available biomarker tests
- The median time from diagnosis to first-line therapy is about five weeks
Data from Protocol 1 will be compared to Protocol 2, which will prospectively evaluate contemporary ordering patterns and turnaround times. It will enroll about 1,000 patients from 11 sites across The Network and will monitor the real-world patient journey from presentation through their first line of cancer therapy, focusing on how diagnostic biomarker information is obtained, utilized and operationalized in decision-making. Patients are currently being enrolled in this stage of the study.
In addition to recognizing the progress that’s been made through this innovative research, I want to acknowledge the growing number of consortium participants and welcome two new life science companies. Genentech and AstraZeneca have joined this collaborative effort along with current members Amgen, Eli Lilly and Company and Mirati Therapeutics.
We will continue to grow the MYLUNG Consortium to reach up to 7,500 patients from approximately 20 Network sites over a five-year period during Protocol 3, integrating findings from the previous protocols and exploring new processes and associated outcomes. Thank you to the participating physicians and patients – together we are enabling providers to make the best treatment recommendations while improving access to testing and therapies for patients with lung cancer.
For more information, visit the MYLUNG webpage and blog on usoncology.com
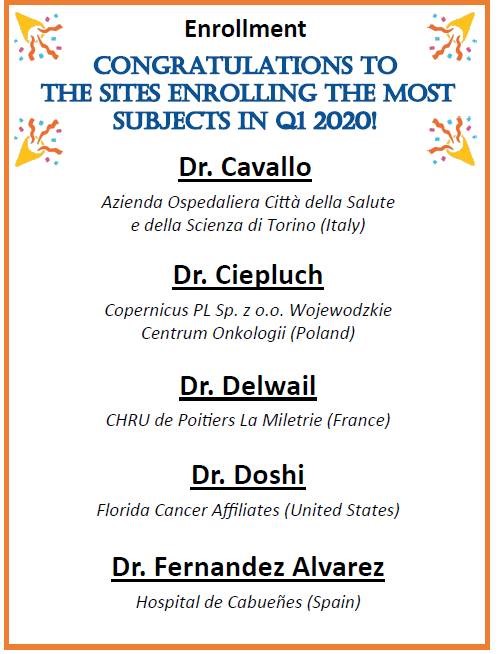
TOP ENROLLING CLINICAL TRIAL SITE IN THE UNITED STATES
Congratulation to Dr. Ketan Doshi and the research team at Ocala Oncology/Florida Cancer Affiliates for being recognized as the top enrolling site in the United States for a Follicular Lymphoma study evaluating patients receiving the combination of Ibrutinib and Rituximab for the treatment of follicular lymphoma. View Clinical Trials
Melanoma Treatment Options
Different types of treatment are available for patients with melanoma. These are the five treatment options commonly used for melanoma depending on the stage of the cancer.
Surgery
Surgery to remove the tumor is the primary treatment of all stages of melanoma. The doctor may remove the tumor as well as check to see if the cancer has spread to the lymph system.
- Wide local excision: Surgery to remove the melanoma and some of the normal tissue around it. Some of the lymph nodes may also be removed.
- Lymphadenectomy: A surgical procedure in which the lymph nodes are removed and a sample of tissue is checked under a microscope for signs of cancer.
- Sentinel lymph node biopsy: The removal of the sentinel lymph node (the first lymph node the cancer is likely to spread to from the tumor) during surgery. A radioactive substance and/or blue dye is injected near the tumor. The substance or dye flows through the lymph ducts to the lymph nodes. The first lymph node to receive the substance or dye is removed. A pathologist views the tissue under a microscope to look for cancer cells. If cancer cells are not found, it may not be necessary to remove more lymph nodes.
Skin grafting (taking skin from another part of the body to replace the skin that is removed) may be done to cover the wound caused by surgery.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body. This is called systemic chemotherapy.
When chemotherapy is placed directly into the spinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas. This is regional chemotherapy.
One type of regional chemotherapy used for melanoma patients is used to inject the anticancer drugs directly to the arm or leg the cancer is in. The flow of blood to and from the limb is temporarily stopped with a tourniquet. A warm solution with the anticancer drugs is put directly into the blood of the limb. This gives a high dose of drugs to the area where the cancer is.
The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Even if the doctor removes all the melanoma during surgery, there can be some left that can’t be seen. Some patients may be offered chemotherapy after surgery to kill any cancer cells that are left. Chemotherapy given after surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
Biologic Therapy
Biologic therapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This type of cancer treatment is also called biotherapy or immunotherapy.
- Interferon and interleukin-2 (IL-2) are types of biologic therapy used to treat melanoma. Interferon affects the division of cancer cells and can slow tumor growth. IL-2 boosts the growth and activity of many immune cells, especially lymphocytes (a type of white blood cell). Lymphocytes can attack and kill cancer cells.
- Tumor necrosis factor (TNF) therapy is a type of biologic therapy used with other treatments for melanoma. TNF is a protein made by white blood cells in response to an antigen or infection. Tumor necrosis factor can be made in the laboratory and used as a treatment to kill cancer cells.
Targeted Therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. The following types of targeted therapy are being used in the treatment of melanoma:
- Monoclonal antibody therapy: A cancer treatment that uses antibodies made in the laboratory, from a single type of immune system cell. These antibodies can identify substances on cancer cells or normal substances that may help cancer cells grow. The antibodies attach to the substances and kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells. Monoclonal antibodies may be used with chemotherapy as adjuvant therapy. Ipilimumab is a monoclonal antibody used to treat melanoma.
- Signal transduction inhibitors: A substance that blocks signals that are passed from one molecule to another inside a cell. Blocking these signals may kill cancer cells. Vemurafenib is a signal transduction inhibitor used to treat advanced melanoma or tumors that cannot be removed by surgery.
- Oncolytic virus therapy: A type of targeted therapy that is being studied in the treatment of melanoma. Oncolytic virus therapy uses a virus that infects and breaks down cancer cells but not normal cells. Radiation therapy or chemotherapy may be given after oncolytic virus therapy to kill more cancer cells.
- Angiogenesis inhibitors: A type of targeted therapy that is being studied in the treatment of melanoma. Angiogenesis inhibitors block the growth of new blood vessels. In cancer treatment, they may be given to prevent the growth of new blood vessels that tumors need to grow.
Physician Search Results
Location Search Results
Test Title
body text
Test
boody
Treatment
Treatment for idiopathic thrombocytopenic purpura (ITP) is based on how much and how often you’re bleeding and your platelet count. In some cases, treatment may not be needed. Medicines often are used as the first course of treatment. Treatments used for children and adults are similar. Adults with ITP who have very low platelet counts or problems with bleeding often are treated. Adults who have milder cases of ITP may not need any treatment, other than watching their symptoms and platelet counts.
If adults or children who have ITP need treatment, medicines often are tried first. Corticosteroids, such as prednisone, are commonly used to treat ITP. These medicines, called steroids for short, help increase your platelet count by lowering the activity of your immune system. However, steroids have a number of side effects, and some people relapse (get worse) when treatment ends. The steroids used to treat ITP are different from illegal steroids taken by some athletes to enhance performance. Corticosteroids aren't habit-forming, even if you take them for many years.
Some medicines used to help raise the platelet count are given through a needle inserted into a vein. These medicines include immune globulin and anti-Rh (D) immunoglobulin.
Medicines also may be used along with a procedure to remove the spleen, called splenectomy. If steroids, immunoglobulins, or splenectomy don’t help, two newer medicines—eltrombopag and romiplostim—can be used to treat ITP.
If necessary, the spleen will be removed surgically. This organ is located in the upper left abdomen. The spleen is about the size of a golf ball in children and a baseball in adults. The spleen makes antibodies (proteins) that help fight infection. In ITP, these antibodies destroy platelets. If ITP hasn't responded to steroids, removing the spleen will reduce the destruction of platelets. However, it also may make you more likely to get certain infections. Before you have the surgery, your doctor may give you vaccines to help prevent these infections. If your spleen is removed, your doctor will explain what steps you can take to help avoid infections and what symptoms to watch for.
Some people with ITP who have severe bleeding may need to have platelet transfusions and be hospitalized. Some people will need a platelet transfusion before having surgery. For a platelet transfusion, donor platelets from a blood bank are injected into the recipient's bloodstream. This increases the platelet count for a short time.
Types
There are two types of ITP: acute (temporary or short-term) and chronic (long-lasting).
- Acute ITP generally lasts less than 6 months. It mainly occurs in children, both boys and girls, and is the most common type of ITP. Acute ITP often occurs after an infection caused by a virus.
- Chronic ITP is long-lasting (6 months or longer) and mostly affects adults. However, some teenagers and children can get this type of ITP. Chronic ITP affects women 2 to 3 times more often than men.
Symptoms
People who have ITP often have purple bruises that appear on the skin or on the mucous membranes (for example, in the mouth). The bruises mean that bleeding has occurred in small blood vessels under the skin. A person who has ITP also may have bleeding that results in tiny red or purple dots on the skin. These pinpoint-sized dots are called petechiae. Petechiae may look like a rash. Bleeding under the skin causes the purple, brown, and red color of the petechiae and purpura.
People who have ITP also may have nosebleeds, bleeding from the gums when they have dental work done, or other bleeding that's hard to stop. Women who have ITP may have menstrual bleeding that's heavier than usual.
More extensive bleeding can cause hematomas. A hematoma is a collection of clotted or partially clotted blood under the skin. It looks or feels like a lump. Bleeding in the brain as a result of ITP is very rare, but can be life threatening if it occurs.
In most cases, an autoimmune response is believed to cause ITP. Normally your immune system helps your body fight off infections and diseases. But if you have ITP, your immune system attacks and destroys its own platelets. The reason why this happens isn’t known. ITP can't be passed from one person to another.
Treatment
Treatment of essential thrombocythemia in patients younger than 60 years who have no symptoms and an acceptable platelet count is usually watchful waiting. Treatment of other patients may include the following:
- Chemotherapy
- Anagrelide therapy
- Biologic therapy using interferon alfa
- Platelet apheresis (therapeutic removal of platelets from the blood)
- A clinical trial of a new investigational treatment
Symptoms and Diagnosis
Essential thrombocythemia often does not cause early symptoms. It is sometimes found during a routine blood test called the Complete Blood Count. The following symptoms may be caused by essential thrombocytopenia or by other conditions. A doctor should be consulted if any of these problems occur:
- Headache
- Burning or tingling in the hands or feet
- Redness and warmth of the hands or feet
- Vision or hearing problems
Platelets are sticky. When there are too many platelets, they may clump together and make it hard for the blood to flow. Clots may form in blood vessels and there may also be increased bleeding. These can cause serious health problems such as stroke or heart attack.
Treatment
Treatment of primary myelofibrosis in patients without symptoms is usually watchful waiting. Treatment of primary myelofibrosis in patients with symptoms may include the following:
- Transfusion of red blood cells to relieve symptoms and improve quality of life
- Biologic therapy using interferon alfa or erythropoietic growth factors
- Splenectomy
- Radiation therapy to the spleen
- Chemotherapy
- Donor stem cell transplant
- Thalidomide or lenalidomide
- A clinical trial of a new treatment
Symptoms and Diagnosis
Possible signs of primary myelofibrosis include pain below the ribs on the left side and feeling very tired.
Primary myelofibrosis often does not cause early symptoms. It is sometimes found during a routine blood test. The following symptoms may be caused by primary myelofibrosis or by other conditions. A doctor should be consulted if any of these problems occur:
- Feeling pain or fullness below the ribs on the left side
- Feeling full sooner than normal when eating
- Feeling very tired
- Shortness of breath
- Easy bruising or bleeding
- Petechiae (flat, red, pinpoint spots under the skin that are caused by bleeding)
- Fever
- Night sweats
- Weight loss
- A special blood test is used to diagnose primary myelofibrosis
In addition to a complete blood count, bone marrow aspiration and biopsy, and cytogenetic analysis, a peripheral blood smear is used to diagnose primary myelofibrosis. A peripheral blood smear is a procedure in which a sample of blood is checked for tear drop-shaped red blood cells, the number and kinds of white blood cells, the number of platelets, and the presence of blast cells.
Treatment
Treatment of de novo and secondary myelodysplastic syndromes may include the following:
- Supportive care with transfusion therapy.
- High-dose chemotherapy with stem cell transplant using stem cells from a donor.
- Supportive care with growth factor therapy.
- Chemotherapy with azacitidine, decitabine, or other anticancer drugs.
- Supportive care with drug therapy.
- A clinical trial of a new anticancer drug.
- A clinical trial of low- dose chemotherapy with stem cell transplant using stem cells from a donor.
- A clinical trial of a combination of treatments.
- A clinical trial of growth factor therapy.
Treatment of previously treated myelodysplastic syndromes may include the following:
- High-dose chemotherapy with stem cell transplant using stem cells from a donor.
- Chemotherapy with azacitidine or decitabine.
- Supportive care with transfusion therapy, growth factor therapy, and/or drug therapy.
- A clinical trial of low- dose chemotherapy with stem cell transplant using stem cells from a donor.
- A clinical trial of new drug therapy.
- A clinical trial of a combination of treatments.
-
A clinical trial of growth factor therapy.
Staging
There is no staging system for myelodysplastic syndromes. Treatment is based on whether the disease developed after the patient was exposed to factors that cause myelodysplastic syndrome or whether the disease was previously treated. Myelodysplastic syndromes are grouped for treatment as follows:
- De novo myelodysplastic syndromes develop without any known cause.
- Secondary myelodysplastic syndromes develop after the patient was treated with chemotherapy or radiation therapy for other diseases or after being exposed to radiation or certain chemicals that are linked to the development of myelodysplastic syndromes. Secondary myelodysplastic syndromes may be harder to treat than de novo myelodysplastic syndromes.
- Previously treated myelodysplastic syndromes
- The myelodysplastic syndrome has been treated but has not gotten better.
Diagnosis
Tests that examine the blood and bone marrow are used to detect (find) and diagnose myelodysplastic syndromes. The following tests and procedures may be used:
Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
Complete blood count (CBC) with differential: A procedure in which a sample of blood is drawn and checked for the following:
- The number of red blood cells and platelets
- The number and type of white blood cells
- The amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- The portion of the blood sample made up of red blood cells
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions.
Peripheral blood smear: A procedure in which a sample of blood is checked for changes in the number, type, shape, and size of blood cells and for too much iron in the red blood cells.
Cytogenetic analysis: A test in which cells in a sample of blood or bone marrow are viewed under a microscope to look for certain changes in the chromosomes.
Bone marrow aspiration and biopsy: The removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone. A pathologist views the bone marrow, blood, and bone under a microscope to look for abnormal cells.
Myelodysplastic syndromes are diagnosed based on certain changes in the blood cells and bone marrow.
- Refractory anemia: There are too few red blood cells in the blood and the patient has anemia. The number of white blood cells and platelets is normal.
- Refractory anemia with ringed sideroblasts: There are too few red blood cells in the blood and the patient has anemia. The red blood cells have too much iron. The number of white blood cells and platelets is normal.
- Refractory anemia with excess blasts: There are too few red blood cells in the blood and the patient has anemia. Five percent to 19% of the cells in the bone marrow are blasts and there are a normal number of blasts found in the blood. There also may be changes to the white blood cells and platelets. Refractory anemia with excess blasts may progress to acute myeloid leukemia. See the PDQ Adult Acute Myeloid Leukemia Treatment summary for more information.
- Refractory anemia with excess blasts in transformation: There are too few red blood cells, white blood cells, and platelets in the blood and the patient has anemia. Twenty percent to 30% of the cells in the bone marrow are blasts and more than 5% of the cells in the blood are blasts. Refractory anemia with excess blasts in transformation is sometimes called acute myeloid leukemia.
- Refractory cytopenia with multilineage dysplasia: There are too few of at least two types of blood cells. Less than 5% of the cells in the bone marrow are blasts and less than 1% of the cells in the blood are blasts. If red blood cells are affected, they may have extra iron. Refractory cytopenia may progress to acute leukemia.
- Myelodysplastic syndrome associated with an isolated del(5q) chromosome abnormality: There are too few red blood cells in the blood and the patient has anemia. Less than 5% of the cells in the bone marrow and blood are blasts. There is a specific change in the chromosome.
- Unclassifiable myelodysplastic syndrome: There are too few of one type of blood cell in the blood. The number of blasts in the bone marrow and blood is normal, and the disease is not one of the other myelodysplastic syndromes.
Types
There are several types of myelodysplastic syndromes.
Myelodysplastic syndromes have too few of one or more types of healthy blood cells in the bone marrow or blood. Myelodysplastic syndromes include the following diseases:
- Refractory anemia
- Refractory anemia with ringed sideroblasts.
- Refractory anemia with excess blasts.
- Refractory anemia with excess blasts in transformation.
- Refractory cytopenia with multilineage dysplasia.
- Myelodysplastic syndrome associated with an isolated del(5q) chromosome abnormality.
-
Unclassifiable myelodysplastic syndrome.
Diseases & Conditions That We Treat
Our expert team of oncology and hematology specialists treat patients with a broad range of cancer types and hematological disorders including those listed below.
Adrenal Cortical Cancer
Anal Cancer
Aplastic Anemia
Bile Duct Cancer
Bladder Cancer
Bone Cancer
Bone Metastasis
Brain and Central Nervous System Tumors
Breast Cancer
Cervical Cancer
Coagulation Disorders
Colon and Rectal Cancer
Deep Vein Thrombosis
Endometrial Cancer
Eye Cancer
Follicular Lymphoma
Gallbladder Cancer
Gastrointestinal Tumors
Gestational Trophoblastic Disease
Hodgkin's Disease
Immune Thrombocytopenic Purpura
Kidney Cancer
Laryngeal and Hypopharyngeal Cancer
Leukemia
Liver Cancer
Lung Cancer
Male Breast Cancer
Malignant Mesothelioma
Multiple Myeloma
Myelodysplastic Syndrome
Nasal Cavity and Paranasal Cancer
Nasopharyngeal Cancer
Neuroblastoma
Non-Hodgkin’s Lymphoma
Oral Cavity and Oropharyngeal Cancer
Osteosarcoma
Ovarian Cancer
Pancreatic Cancer
Pituitary Tumor
Prostate Cancer
Retinoblastoma
Rhabdomyosarcoma
Salivary Gland Cancer
Sarcoma
Stomach Cancer
Testicular Cancer
Thrombocytopenia
Thymus Cancer
Thyroid Cancer
Patient Support Groups
Studies have shown that support groups are very beneficial for the survival and quality of life for cancer patients, their families and caregivers. The following resources are available to cancer patients and their families in the Ocala area:
Cancer Resource Room
Located in the Florida Cancer Affiliates' Main Ocala office, this room offers patients an array of free products for their cancer journey, including wigs, blankets, hats, port covers, pillows and more. This is open to the public for anyone that has a need because of cancer. 433 SW 10th Street in Ocala.
Sisterhood Of Survivors
This is a monthly meeting for breast cancer survivors to share their experience and be informed and educated on treatments and treatments available during their journey. This is offered the LAST Tuesday of each month at 1:00 pm at Ocala West United Church, 9330 SW 105th Street in Ocala. For more information, contact 352-291-6904.
Cancer Education Series
The Cancer Alliance of Marion County offers quarterly educational programs to inform medical professions and patients of the many aspects of cancer care. There will be an opportunity to mingle as both patients and professionals share knowledge and insight together. Seating is limited and dinner is provided. For more information, contact 352-401-1534
Multiple Myeloma – You are not alone!
Support group for all interested patients, care givers, family members and friends are encouraged to join. The Stomping Out Myeloma Support Group meets every second Saturday of each month at 11:00am at the Howard Academy, 306 NW 7th Avenue in Ocala. For more information, please contact 352-671-3060.
Cancer Support Group
Share your cancer stories and bond with others going through the cancer journey. This cancer support group meets the 4th Friday of each month at 1:30 in the Advent Health Ocala Auxilliary Building. 1542 SW 1st Avenue, Ocala. Please contact Laura at 352-690-5675 for more information.
Particpants in these groups support each other, identify with one another, and gain some added strength from a relaxed comfortable group setting. During these meetings, participants are encouraged to vent their feelings and share their experiences, but coming to listen can often be helpful too. Participants continually experience many healing connections and positive experiences during this important time together.
Helpful Websites
When a person first learns that they have cancer or a blood disorder/disease the primary concern is survival. As treatment begins, however, new issues become more important. Some of these include relationships with others, side effects from treatments, and nutrition and diet.
Living with cancer or a blood disease/disorder is challenging, and it is best to be educated about issues surrounding survival in order to live a full and productive life.
Below are links to websites containing information for people living with cancer or a blood disorder/disease. The content provided through these links is not the information of Florida Cancer Affiliates, nor does the practice necessarily endorse the content. In addition, all content provided through these links is for information only and does not constitute medical advice. Please consult your Florida Cancer Affiliates physician before acting or relying upon such information.
National Organizations
American Cancer Society (ACS)
English
Espanol
American College of Radiation Oncology (ACRO)
http://www.acro.org
American Institute of Cancer Resarch
American Medical Association (AMA)
http://www.ama-assn.org
American Society of Hematology (ASH)
http://www.hematology.org
American Society for Therapeutic Radiology and Oncology (ASTRO)
http://www.astro.org
American Society of Clinical Oncology (ASCO)
http://www.asco.org
Association of Cancer Online Resources (ACOR)
http://www.acor.org
CancerEducation.com
http://www.cancereducation.com
Cancer News on the Net®
http://www.cancernews.com
Cancer Research Institute (CRI)
http://www.cancerresearch.org
Cancer.net
http://www.cancer.net
CancerGuide
http://www.cancerguide.org
Healthfinder
http://www.healthfinder.gov
Medline Plus
http://www.nlm.nih.gov/medlineplus
Myelodysplastic Syndromes Foundation
www.mds-foundation.org
National Alliance for Caregiving (NAC)
http://www.caring.org
National Cancer Institute (NCI)
English
Espanol
National Comprehensive Cancer Network (NCCN)
http://www.nccn.org
Needy Meds
http://www.needymeds.com
National Institutes of Health (NIH)
http://www.nih.gov
National Library of Medicine (NLM)
http://www.nlm.nih.gov
OncoLink (University of Pennsylvania)
http://www.oncolink.org
Oncology Nursing Society (ONS)
http://www.ons.org
Planet Cancer
http://www.planetcancer.org
Quackwatch
http://www.quackwatch.com
Society of Gynecologic Oncologists
http://www.sgo.org
U.S. Food and Drug Administration (FDA)
http://www.fda.gov
US Oncology
http://www.usoncology.com
Disease-Specific Organizations
National Brain Tumor Society
http://www.braintumor.org
BreastCancer.org
http://www.breastcancer.org
Breast Cancer Network of Strength
(formerly Y-ME National Breast Cancer Organization)
http://www.networkofstrength.org
Colon Cancer Alliance
http://www.ccalliance.org
Leukemia & Lymphoma Society
http://www.leukemia-lymphoma.org
Lung Cancer Alliance
http://www.lungcanceralliance.org
Lymphoma Research Foundation
http://www.lymphoma.org
The Mesothelioma Center
http://asbestos.com
Mesothelioma Guide
http://www.mesotheliomaguide.com/
Ovarian Cancer National Alliance
http://www.ovariancancer.org
National Ovarian Cancer Coalition
http://www.ovarian.org
Prostate Cancer Foundation
http://www.pcf.org
Skin Cancer Foundation
http://www.skincancer.org
Patient Advocacy/Survivorship
National Coalition for Cancer Survivorship
http://www.canceradvocacy.org
Cancer Survivors Network
csn.cancer.org
National Cancer Survivor Day® Foundation, Inc.
http://www.ncsdf.org
National Patient Advocate Foundation (NPAF)
http://www.npaf.org
Patient Advocate Foundation
http://www.patientadvocate.org
Patient & Family Support Services
Caring Connections
http://www.caringinfo.org
Gilda’s Club Worldwide
http://www.gildasclub.org
Lance Armstrong Foundation
http://www.livestrong.org
Life Beyond Cancer Foundation
http://www.lifebeyondcancer.org
Look Good…Feel Better
English
Espanol
National Center for Complementary and Alternative Medicine
http://www.nccam.nih.gov
National Family Caregivers Association (NFCA)
http://www.nfcacares.org
People Living Through Cancer
http://www.pltc.org
US TOO Prostate Cancer Support Group
http://www.ustoo.com
The Wellness Community
http://www.thewellnesscommunity.org
PET/CT Diagnostic Imaging
Positron Emission Tomography (PET)-Computed Tomography (CT) Scan
Your Florida Cancer Affiliates physician may include PET and CT scans in your cancer care plan, as these tests can greatly improve our ability to evaluate and treat your disease. The PET and CT scan brings two powerful imaging techniques and combines them into one of the most advanced medical imaging tools available. It answers questions such as: where is the tumor, how big is it, is it malignant, benign or due to inflammatory change, and has it spread?
Positron Emission Tomography (PET) shows a body’s metabolic activity, while Computed Tomography (CT) shows anatomy. When fused together, the information from these two scans can be used with a high degree of confidence to detect, localize and assess the exact stage for a variety of cancers.
The scan reveals your body’s metabolic pattern, including both normal and abnormal tissue activity, such as a tumor. At the same time, the CT scan reveals the detailed anatomy of the area where the normal and abnormal activity is taking place. The improved images reduce the number of invasive procedures required during diagnosis and follow up care for most patients.
A PET scan alone is very helpful in showing the presence or spread of many malignant tumors. When it is combined with a CT scan in the same session, our physicians are able to pinpoint the exact location of a tumor, more accurately assess the stage of the disease and follow the progress of each patient’s treatments.
Cancer Screenings
Screening exams can diagnose cancer at the earliest stages, when treatment will be the most effective. Florida Cancer Affiliates recommends that patients have routine screening and/or self-exams for breast, prostate, colorectal, skin, testicular and cervical cancers.
The screening guidelines below offer recommended timing for specific ages, genders, and cancer types.
Adults at Every Age
- Keep an eye on your skin and check for changes in freckles, moles, and other skin markings once a month.
- Women should check their breasts for lumps every month and have a clinical breast exam every one to three years.
- Men should check both testicles for hard lumps or changes in size or shape every month.
- Individuals should be aware of their cancer risk, which may be higher for those with a personal or family history of cancer, or people who have certain genetic profiles that have been associated with specific cancer types. Screening may need to begin at an earlier age for those with these risk factors.
- Research does not indicate the most appropriate age to begin cancer screening. Patients should consult their physicians to make an informed decision about screening, considering the patient's history and circumstances.
20s
- All women should have a Pap test to screen for cervical cancer at least once every year beginning at age 21, or approximately three years after a woman begins having sexual intercourse, whichever comes first, regardless of whether they have received the human papillomavirus (HPV) vaccine.
30s
- Women in their 30s should have annual Pap tests, but women with three consecutive normal Pap tests may limit screenings to every two or three years. Women should also consider a DNA HPV test, which, given in conjunction with a routine Pap test, may identify existing HPV infections that could lead to cervical cancer.
- Women with a high risk for breast cancer (greater than 20 percent) associated with defined genetic profiles or family history should discuss with their physician the use of MRI for screening, in combination with a yearly mammogram. MRI screenings can help detect breast cancer in younger women with dense breast tissue.
40s
- Women age 40 and older should begin having an annual mammogram, clinical breast exam, and if recommended by their physician, an MRI screening.
- Women in their 40s should continue to have annual Pap tests, but women with three consecutive normal Pap tests may limit screenings to every two or three years. Women may also consider a DNA HPV test.
- Men with a high risk of prostate cancer (African Americans and men with a family history of prostate cancer before age 65) should discuss with their physicians whether screenings are appropriate beginning at age 45.
- Men with a higher risk of prostate cancer (those with several immediate family members with prostate cancer) should discuss screenings with their physicians beginning at age 40.
- Men and women with increased risk factors for colorectal cancer should discuss with their physicians whether to begin screenings earlier than the normal age 50.
50s
- Women age 50 and older should continue having an annual mammogram, clinical breast exam, and if recommended by their physician, an MRI screening.
- Women in their 50s should continue to have annual Pap tests, but women with three consecutive normal Pap tests may limit screenings to every two or three years. Women may also consider a DNA HPV test.
- Beginning at age 50, men should discuss with their physicians the benefits and risks associated with prostate cancer screening to determine if it is right for them. Prostate cancer screening may involve a prostate-specific antigen (PSA) blood test and a digital rectal examination (DRE).
-
Beginning at 50, both men and women should begin screening for colorectal cancer with one of the following options:
- Annual fecal occult blood tests (FOBT) or fecal immunochemical tests (FIT)
- Every five years, a flexible sigmoidoscopy
- Every five years, a double-contrast barium enema
- Every 10 years, a colonoscopy
Finding Patient Support
At Florida Cancer Affiliates, we encourage and connect patients and their families with the best supportive services for all the educational, emotional and financial challenges they may be facing at this difficult time.
If you have cancer and are undergoing cancer treatment, there are places in our community that offer additional help. There are many local organizations throughout the country that offer a variety of practical support services to patients with cancer.
Many of the national cancer organizations, such as the American Cancer Society, can assist you in finding additional support services in your area.
Visit our Helpful Websites page for more information, or call our practice at any time and we will be glad to assist you.
Clinical Research Overview
Advancing Cancer Care through Clinical Trials
Florida Cancer Affiliates has embraced clinical trial research as a critical component of community-based care for our patients with cancer or blood disorders. Participating in clinical trials shows us what works (and what doesn't) in medicine. Plus, they are the best way for our doctors to learn what is safe and effective in treating diseases such as cancer.
Clinical research offers us access to new investigational drugs (not always available to the general public); it reduces treatment-related side effects and introduces new methods of care for our patients.
We access clinical trials through our affiliation with The US Oncology Research Network, one of the nation's largest healthcare networks dedicated to cancer treatment and clinical trial research, specializing in Phase I-IV clinical trials. This affiliation allows us to provide patients in the communities that we serve, access to many of the most current and innovative clinical trials available. The US Oncology Research Network has contributed to the development of 39 anti-cancer drugs approved by the FDA.
If you would like more information, please ask your physician about available clinical trials that might be suitable for you.
Is a Clinical Trial Right for You?
Is a Clinical Trial Right for You?
Below is a list of questions that you might have when discussing clinical trials with your Ocala Oncology/Florida Cancer Affiliates physician. If you express an interest in a clinical trial, we will explain the research trial process, and address any questions you might have prior to starting any research procedures in a process known as Informed Consent.
The Informed Consent discussion should address many of the questions below, and is an opportunity for you to have your questions answered prior to deciding to participate in a clinical trial.
- How will the clinical trial help me?
- What other treatment options are available?
- What side effects might I experience?
- Are there possible long-term risks?
- How will participating in this study affect my daily life?
- Who is sponsoring this study?
- What kinds of treatment, medical tests or procedures will I have during the study? How often?
- Where will I receive my treatment?
- Who will be in charge of my care?
- How long will the study last?
- Will I have to pay for any treatments, tests, or other charges?
- Will my health insurance cover treatments and tests I receive as part of this study?
- How am I protected?
- What kind of follow-up care will I receive after the study?
- When do I have to make a decision about participation?
If you have any questions or need more information about your treatment or research studies currently in progress, please let us know.
For more information on clinical trials, visit The US Oncology Network Clinical Trials page or the National Cancer Institute.
How Targeted Cancer Therapies Work for Patients
Targeted cancer therapies interfere with cancer cell division and growth in many different ways. Some of these therapies focus on proteins that are involved in cell messaging pathways, which form a complicated communication process that directs basic cellular functions and activities, such as cell division, cell movement, how a cell responds to different outside stimuli, and even cell death.
Targeted cancer therapies block these bad signals that tell cancer cells to grow and divide uncontrollably. By doing this, the therapies can help stop cancer development and can cause cancer cell death through a process known as apoptosis.
Other targeted therapies can cause cancer cell death by actually making apoptosis happen. Sometimes it happens indirectly, by boosting a patient’s immune system to see and kill cancer cells, and bringing the deadly ingredients right to them.
To learn more and to see what types of cancer are currently being treated with targeted therapies, visit the National Cancer Institute.
Idiopathic Thrombocytopenic Purpura (ITP)
Idiopathic thrombocytopenic purpura (ITP) is a bleeding condition in which the blood doesn't clot as it should. This is due to a low number of blood cell fragments called platelets. Platelets also are called thrombocytes which are made in your bone marrow along with other kinds of blood cells. Platelets stick together (clot) to seal small cuts or breaks on blood vessel walls and stop bleeding. "Idiopathic" means that the cause of the condition isn't known. "Thrombocytopenic" means there's a lower than normal number of platelets in the blood. "Purpura" refers to purple bruises caused by bleeding under the skin.
**All information about ITP is provided by the National Heart, Lung, and Blood Institute as a part of the National Institutes of Health and the U.S. Department of Health and Human Services
Blood Clots or Excessive Bleeding
Cancer Care Centers of South Texas is affiliated with the Anticoagulation Clinics of North America (ACNA). ACNA is a complete anticoagulation and thrombosis management service providing high-quality, efficient care to patients receiving anticoagulation with warfarin (Coumadin) and antithrombotic medications (blood thinners and platelet inhibitors).
Services offered include both out-patient and in-hospital management of anticoagulant medications. In addition, ACNA offers a comprehensive out-patient treatment program for Deep Vein Thrombosis (DVT) and comprehensive evaluation and management of patients with thrombotic disorders. Most patients with deep vein thrombosis can now be evaluated and treated in our office without needing a hospital admission.
For extensive information about our anticoagulation and thrombosis management service, please see our complete website for the Anticoagulation Clinics of North America.
Primary Myelofibrosis
The bone marrow is made of tissues that make blood cells (red blood cells, white blood cells, and platelets) and a web of fibers that support the blood-forming tissues. In primary myelofibrosis (also called chronic idiopathic myelofibrosis), large numbers of blood stem cells develop into blood cells that do not mature properly (blasts). The web of fibers inside the bone marrow also becomes very thick (like scar tissue) and slows the blood-forming tissue’s ability to make blood cells. This causes the blood-forming tissues to make fewer and fewer blood cells. In order to make up for the low number of blood cells made in the bone marrow, the liver and spleen begin to make the blood cells.
Essential Thrombocythemia
Essential thrombocythemia is a disease in which too many platelets (thrombocytes) in the blood. This abnormal increase in the number of platelets in the blood is due to increased production by the bone marrow.
Treatment
The purpose of treatment for polycythemia vera is to reduce the number of extra blood cells. Treatment of polycythemia vera may include the following:
- Phlebotomy (removing a therapeutic level of blood)
- Chemotherapy with or without phlebotomy
- Biologic therapy using interferon alfa
- Low- dose aspirin
A clinical trial of a new treatment.
Treatment
The purpose of treatment for polycythemia vera is to reduce the number of extra blood cells. Treatment of polycythemia vera may include the following:
- Phlebotomy (removing a therapeutic level of blood)
- Chemotherapy with or without phlebotomy
- Biologic therapy using interferon alfa
- Low- dose aspirin
- A clinical trial of a new treatment.
Symptoms & Diagnosis
Possible signs of polycythemia vera include headaches and a feeling of fullness below the ribs on the left side.
Polycythemia vera often does not cause early symptoms. It is sometimes found during a routine blood test. Symptoms may occur as the number of blood cells increases. Other conditions may cause the same symptoms. A doctor should be consulted if any of the following problems occur:
- A feeling of pressure or fullness below the ribs on the left side
- Headaches
- Double vision or seeing dark or blind spots that come and go
- Itching all over the body, especially after being in warm or hot water
- Reddened face that looks like a blush or sunburn
- Weakness
- Dizziness
- Weight loss for no known reason
Special blood tests are used to diagnose polycythemia vera. In addition to a complete blood count, bone marrow aspiration and biopsy, and cytogenetic analysis, a serum erythropoietin test is used to diagnose polycythemia vera. In this test, a sample of blood is checked for the level of erythropoietin (a hormone that stimulates new red blood cells to be made).
Polycythemia Vera
Polycythemia vera is a disease in which too many red blood cells are made in the bone marrow.
In polycythemia vera, the blood becomes thickened with too many red blood cells. The number of white blood cells and platelets may also increase. These extra blood cells may collect in the spleen and cause it to swell. The increased number of red blood cells or platelets in the blood can cause bleeding problems and make clots form in blood vessels. This can increase the risk of stroke or heart attack. In patients who are older than 65 years or who have a history of blood clots, the risk of stroke or heart attack is higher. Patients also have an increased risk of developing acute myeloid leukemia or primary myelofibrosis.
Myelodysplastic Syndromes
Myelodysplastic syndromes are a group of diseases in which the bone marrow does not make enough healthy blood cells.
Myelodysplastic syndromes are diseases of the blood and bone marrow. Normally, the bone marrow makes blood stem cells (immature cells) that develop into mature blood cells over time. A blood stem cell may become a myeloid stem cell or a lymphoid stem cell. The lymphoid stem cell develops into a white blood cell. The myeloid stem cell develops into one of three types of mature blood cells:
- Red blood cells that carry oxygen and other materials to all tissues of the body.
- White blood cells that fight infection and disease.
- Platelets that help prevent bleeding by causing blood clots to form.
Cancer Care Centers of South Texas have been recognized nationally for expertise in the diagnosis, treatment and research of myelodysplasia and is designated as a "Center of Excellence" by the The Myelodysplastic Syndromes Foundation.
Lo que usted necesita saber sobre síndromes mielodisplásicos.
Event Speakers
Expert Speakers Available
Need a presenter for a medical event?
Our physicians are available for speaking engagements.
Phone Call Guide
Please use this guide for when you should call our office:
Call during regular office hours (Monday-Friday) for non-urgent issues including:
- If you have to schedule or reschedule an appointment
- If you have questions about your medication, treatment or side effects
- If you’re having nutrition problems
- If you need a prescription refill order for your pharmacy
- Please call by 3 p.m. and have your pharmacy’s phone number
- For narcotics such as MS Contin or Oxycontin, please plan to come into the office for a written prescription. By law, your pharmacy must have a written prescription and these prescriptions cannot be called into a pharmacy via phone. No narcotic prescriptions can be written on weekends.
- Your comfort and concerns are important to us. If a certain medication is not working, call and let us know.
Call anytime day or night if:
- Fever 100.5 F. degrees or greater
- Uncontrollable nausea or diarrhea
- Pain medication is not working
- Chest pains or shortness of breath
- Severe shaking or chills
- Bleeding from the nose or gums
- Blood in the urine
- Black, tarry bowel movement
- Severe diarrhea
- Constipation with intense abdominal cramping
- Changes in your vision or hearing
- Increased bruising or pinpoint red or purple spots anywhere on the body
- Or any new symptom causing you concern call again, and if any of these symptoms escalate to a life-threatening emergency or an urgent medical condition, call 911. Call our office only after you have made arrangements to get to the Emergency Room.
After Hours Calls
If your call is received after business hours (after 5 p.m.), or on weekends or holidays, the physician on call will be paged on your behalf and will respond quickly. Since your call may not be returned by your personal physician, please be prepared to provide the following information:
- Your diagnosis
- Your chemotherapy drugs
- Your temperature
- Your pharmacy phone number
Please indicate in your phone message:
- Reason for your call
- Full name (spelling of your last name)
- Date of birth
- Best phone number, day and time to reach you
- Name of your oncologist / hematologist
Emergencies or Urgent Calls
If you experience a life-threatening medical emergency, immediately call 911. Upon arrival at the emergency room, ask the staff to call your Florida Cancer Affiliates physician.
If you feel that you need immediate consultation, or advice regarding a serious condition, do not hesitate to call us at 1 (855) 451-7095 during regular business hours, Monday-Friday, 8:30am-5pm. Our clinical staff and physicians return patient calls during business hours between appointments and consultations. If your question is urgent, please tell our telephone operator, so that a provider or nurse can confer with you more promptly.
Please understand that calls for test results and prescription refills will be returned after urgent patient needs are met. All calls are returned in the order of medical priority.
The US Oncology Network
Ocala Oncology/Florida Cancer Affiliates is a practice in The US Oncology Network (The Network). This collaboration unites the practice with more than 1,200 independent physicians dedicated to delivering value-based, integrated care to patients — close to home.
Through The Network, these independent doctors come together to form a community of shared expertise and resources dedicated to advancing local cancer care and to delivering better patient outcomes. The Network is supported by McKesson Corporation, whose coordinated resources and infrastructure allow doctors in The Network to focus on the health of their patients, while McKesson focuses on the health of their practices.
Ocala Oncology/Florida Cancer Affiliates also participates in clinical trials through US Oncology Research, which has played a role in more than 100 FDA-approved cancer therapies, approximately one-third of all cancer therapies approved by the FDA to date. For more information, visit usoncology.com
Why Florida Cancer Affiliates
Our Promise to Our Patients
We appreciate that you are considering partnering with us on this very personal journey. As an important part of your care team, we commit to you:
- To keep you, the person, not your cancer, as the focus of all that we do for you
- To listen to your questions and concerns and help you find the answers you need
- To respect your values, preferences and expressed needs
- To provide you with the information and the understanding that you need to make choices about your care
- To make available to you research advances for providing optimum cancer care
- To provide for both your physical comfort and your emotional support
- To remember that cancer can affect your family and loved ones as well
- To simplify the steps that have to happen for you to receive the best care
Breast Conservation Therapy
Most patients diagnosed with early stage breast cancer have the option to save their breast by choosing breast conservation therapy. New treatment approaches have increased the choices available to women, in some cases eliminating the need for six weeks of traditional external beam radiation, and improving the patient’s quality of life.
The combination of lumpectomy and radiation therapy is commonly called breast-conserving therapy. Lumpectomy is the removal of the breast tumor (the "lump") and some of the normal tissue that surrounds it performed in a "breast conservation or preservation" manner.
Stereotactic Radio Surgery/Stereotactic Body Radiation
Stereotactic Body Radiation Therapy for Lung Cancer is a highly focused form of radiation therapy that offers patients with early stage cancer a greater than 90% chance of success (local control) using a limited number of treatments (usually 5 days). For more advanced disease, a combination of radiation therapy, chemotherapy, and surgery may be utilized to optimize the chance of cure.
Stereotactic Body Radiation Therapy and Stereotactic Radio Surgery have great potential for improved outcomes as highlighted for Lung but must be executed with care and caution in a highly coordinated environment lead by board-certified radiation oncologists experienced with advanced treatment techniques.
Advanced Technology supporting the radiation team is the ELEKTA Infinity linear accelerator with the Agility 160 MLC. Florida Cancer Affiliates is the only oncology treatment center in the area utilizing 4D-CBCT guidance technology for daily Stereotactic Body Radiation Therapy/Stereotactic Radio Surgery treatment. This is critical technology when considering motion of lung tumors caused by breathing motion.
The ELEKTA Infinity supports External beam radiation therapy (EBRT) the most common form of radiotherapy using techniques such as 2D, 3D, IMRT (Intensity Modulated) or electrons to effectively treat a wide range of cancers such as Head and Neck, Breast Prostate, Lung and skin to name just a few. Stereotactic Radio Surgery is a unique form of EBRT that is precisely focused on a tumor within the brain that can be delivered a high dose in a single treatment while sparing normal brain tissue.
Stereotactic Body Radiation Therapy is a treatment procedure similar to Stereotactic Radio Surgery, except that it deals with tumors outside of the CNS such as Lung.
Radiation Therapy
Florida Cancer Affiliates offers advanced radiation therapy technologies. These powerful, targeted, cancer-fighting treatments:
- Provide customized treatment for precise radiation doses
- Lessen harm to surrounding tissue and normal cells
- Reduce treatment times and discomfort
- Minimize side effects
- Increase treatment effectiveness
Radiation therapy may be delivered both externally and internally. Internal radiation, or brachytherapy, places a small amount of radioactive material (seeds) in or near the cancer. External radiation delivers high-energy rays directly at the cancer from a machine outside the body.
Florida Cancer Affiliates offers innovative radiation therapy technologies including:
Overview
Bringing Each Patient the Best Care They Need Today
At Florida Cancer Affiliates, we are committed to providing patients with the best and most advanced, compassionate and comprehensive care available. We begin by offering the most current therapies proven to be effective, using the most advanced diagnostic and treatment technologies.
We continually evaluate the latest advances and proven treatments and identify a treatment plan that meets each patient’s individual needs. We consider many factors, including your medical history, current health, and risks and benefits of various treatment options.
When discussing your treatment options, we will tell you our goals and expected results for the treatment, as well as what can be expected during the treatment process. We find this type of clear communication is mutually beneficial and appreciated by our patients.
Overview
Bringing the Best in Care to You
At Florida Cancer Affiliates, we are committed to providing you with the best and most advanced, complete care available. We begin by offering therapies proven to be effective and advanced diagnostic and treatment technologies. We continue by providing unprecedented access to new investigational drugs through clinical trials.
To us, providing the best care means understanding that having cancer is difficult for patients and their families. Our physicians and staff are kind and compassionate, and will do whatever it takes to make everyone more at ease. From convenient parking to warm and friendly surroundings, our state-of-the-art centers are designed to make our patients comfortable. We believe care should be both advanced and compassionate.
We are leading the way to better care for patients with cancer or blood disorders by participating in many clinical trials that test new drugs, unique approaches to chemotherapy and radiation therapy, or various combinations of treatments. Not only does this push progress and advance cancer treatment, but it gives many of our patients the opportunity to receive promising new therapies and investigational drugs not yet available to patients outside these clinical trials.
Our Mission
National Expertise. Close to Home.
Florida Cancer Affiliates is united in healing nationally with The US Oncology Network, one of the nation’s largest community-based cancer treatment and research networks. This means you have access to physicians who are connected nationwide, providing you with the most advanced therapies and treatment options, including unprecedented investigational drugs through clinical trials, close to home.
Expert Physicians. Exceptional Care.
At Florida Cancer Affiliates, we provide the most advanced and personalized care to patients. Our team includes board certified Medical Oncology, Hematology, and Radiation Oncology physician specialists working together with oncology certified nurses, and certified radiation, imaging, laboratory and research professionals to provide patients with the best care in Bay, Citrus, Lake, Marion, and Sumter counties.
About The US Oncology Network
Florida Cancer Affiliates is united in healing with The US Oncology Network, one of the nation’s largest community-based cancer treatment and research networks focused on advancing cancer care in America. As an affiliate of The US Oncology Network, Florida Cancer Affiliates is united with more than 1,000 physicians and 10,000 cancer professionals nationwide.
The US Oncology Network
The US Oncology Network is one of the largest community-based networks of doctors and practices in the country focused on cancer treatment and research. Each year, the more than 1,000 physicians in The Network touch the lives of more than 850,000 cancer patients in more than 540 locations and more than 80 integrated cancer centers throughout the United States.
Our pioneering, integrated approach to cancer care means that each patient’s cancer care team — medical oncologist, radiation oncologist and surgeon — collaborates to ensure delivery of the highest-quality and most advanced care to patients in the communities where they live.
US Oncology Research
US Oncology Research is the nation’s largest community-based research network specializing in Phase I through Phase IV oncology clinical trials. The investigator- and sponsor-initiated trials bring innovative therapies to patients in local communities across the nation. At any given time, we have more than 200 active clinical trials. We support 14 sites that offer Phase I trials, including first-in-human trials. Our research network has played a role in the development of 43 new cancer therapies approved by the FDA. To date, more than 49,000 patients have participated in our clinical trials, helping to advance the science of cancer care.
Patient Advocacy
The US Oncology Network believes that all cancer patients should have access to the care they need without the threat of severe financial hardship. Patients are offered dedicated support to help access reimbursement- assistance programs. Since the program began in 2006, more than 25,000 patients from across the country received more than $150 million in financial assistance for needed therapies. We work with federal, state and local legislators, as well as government and private payers to foster a greater understanding about oncology patient care and the vital role community oncology practices play in the lives of cancer patients and their families.
Integrated Cancer Care
The US Oncology Network’s pioneering, integrated approach to cancer care means that each patient’s cancer care team — medical oncologist, radiation oncologist and surgeon — collaborates to ensure delivery of the highest-quality and most advanced care to patients in the communities where they live.
Patients respond best to treatment when they receive integrated care close to home, relying on the support of family and friends and keeping their daily routines throughout the treatment process.
We are committed to giving patients access to the highest-quality, most advanced care close to home. Our 541 practice locations in The Network and more than 80 comprehensive cancer centers nationwide mean you can stay near your family and friends and keep your daily routine throughout your treatment process.
For more information, visit www.usoncology.com.
Locations & Physicians
Pancreatic Cancer Staging
Staging is a careful attempt to find out the following:
- The size of the tumor in the pancreas
- Whether the tumor has invaded nearby tissues
- Whether the cancer has spread, and if so, to what parts of the body
When cancer of the pancreas spreads, the cancer cells may be found in nearby lymph nodes or the liver. Cancer cells may also be found in the lungs or in fluid collected from the abdomen.
When cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the original (primary) tumor. For example, if pancreatic cancer spreads to the liver, the cancer cells in the liver are actually pancreatic cancer cells. The disease is metastatic pancreatic cancer, not liver cancer. It’s treated as pancreatic cancer, not as liver cancer. Doctors sometimes call the new tumor in the liver “distant” disease.
To learn whether pancreatic cancer has spread, your doctor may order CT scans or EUS.
Also, a surgeon may look inside your abdomen with a laparoscope (a thin, tube-like device that has a light and a lens for seeing inside the body). The surgeon inserts the laparoscope through a small incision in your belly button. The surgeon will look for any signs of cancer inside your abdomen. You’ll need general anesthesia for this exam.
These are the stages of cancer of the pancreas:
- Stage I: The tumor is found only in the pancreas.
- Stage II: The tumor has invaded nearby tissue but not nearby blood vessels. The cancer may have spread to the lymph nodes.
- Stage III: The tumor has invaded nearby blood vessels.
- Stage IV: The cancer has spread to a distant organ, such as the liver or lungs.
Pancreatic Cancer Treatment Options
Treatment options for people with cancer of the pancreas are surgery, chemotherapy, targeted therapy, and radiation therapy. You’ll probably receive more than one type of treatment.
The treatment that’s right for you depends mainly on the following:
- The location of the tumor in your pancreas
- Whether the disease has spread
- Your age and general health
At this time, cancer of the pancreas can be cured only when it’s found at an early stage (before it has spread) and only if surgery can completely remove the tumor. For people who can’t have surgery, other treatments may be able to help them live longer and feel better.
You may have a team of specialists to help plan your treatment. Specialists who treat cancer of the pancreas include surgeons, medical oncologists, radiation oncologists, and gastroenterologists.
Your health care team can describe your treatment choices, the expected results of each, and the possible side effects. Because cancer treatments often damage healthy cells and tissues, side effects are common. These side effects depend on many factors, including the type and extent of treatment. Side effects may not be the same for each person, and they may even change from one treatment session to the next. Before treatment starts, ask your health care team about possible side effects and how treatment may change your normal activities. You and your health care team can work together to develop a treatment plan that meets your needs.
Surgery
Surgery may be an option for people with an early stage of pancreatic cancer. The surgeon usually removes only the part of the pancreas that has cancer. But, in some cases, the whole pancreas may be removed.
The type of surgery depends on the location of the tumor in the pancreas. Surgery to remove a tumor in the head of the pancreas is called a Whipple procedure. The Whipple procedure is the most common type of surgery for pancreatic cancer. You and your surgeon may talk about the types of surgery and which may be right for you.
In addition to part or all of your pancreas, the surgeon usually removes the following nearby tissues:
- Duodenum
- Gallbladder
- Common bile duct
- Part of your stomach
Also, the surgeon may remove your spleen and nearby lymph nodes.
Surgery for pancreatic cancer is a major operation. You will need to stay in the hospital for one to two weeks afterward. Your health care team will watch for signs of bleeding, infection, or other problems. It takes time to heal after surgery, and the time needed to recover is different for each person. You may have pain or discomfort for the first few days. It’s common to feel weak or tired for a while. You may need to rest at home for one to three months after leaving the hospital.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. Most people with pancreatic cancer get chemotherapy. For early pancreatic cancer, chemotherapy is usually given after surgery, but in some cases, it’s given before surgery. For advanced cancer, chemotherapy is used alone, with targeted therapy, or with radiation therapy.
Chemotherapy for pancreatic cancer is usually given by vein (intravenous). The drugs enter the bloodstream and travel throughout your body. Chemotherapy is given in cycles. Each treatment period is followed by a rest period. The length of the rest period and the number of cycles depend on the anticancer drugs used.
Some drugs used for pancreatic cancer also may cause tingling or numbness in your hands and feet.
Targeted Therapy
People with cancer of the pancreas who can’t have surgery may receive a type of drug called targeted therapy along with chemotherapy.
Targeted therapy slows the growth of pancreatic cancer. It also helps prevent cancer cells from spreading. The drug is taken by mouth.
Side effects may include diarrhea, nausea, vomiting, a rash, and shortness of breath.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It can be given along with other treatments, including chemotherapy.
The radiation comes from a large machine. The machine aims beams of radiation at the cancer in the abdomen. You’ll go to a hospital or clinic 5 days a week for several weeks to receive radiation therapy. Each session takes about 30 minutes.
Although radiation therapy is painless, it may cause other side effects. The side effects include nausea, vomiting, or diarrhea. You may also feel very tired.
Pancreatic Cancer Diagnosis
If you have symptoms that suggest cancer of the pancreas, your doctor will try to find out what’s causing the problems. You may have blood or other lab tests. Also, you may have one or more of the following tests:
- Physical exam: Your doctor feels your abdomen to check for changes in areas near the pancreas, liver, gallbladder, and spleen. Your doctor also checks for an abnormal buildup of fluid in the abdomen. Also, your skin and eyes may be checked for signs of jaundice.
- CT scan: An x-ray machine linked to a computer takes a series of detailed pictures of your pancreas, nearby organs, and blood vessels in your abdomen. You may receive an injection of contrast material so your pancreas shows up clearly in the pictures. Also, you may be asked to drink water so your stomach and duodenum show up better. On the CT scan, your doctor may see a tumor in the pancreas or elsewhere in the abdomen.
- Ultrasound: Your doctor places the ultrasound device on your abdomen and slowly moves it around. The ultrasound device uses sound waves that can’t be heard by humans. The sound waves make a pattern of echoes as they bounce off internal organs. The echoes create a picture of your pancreas and other organs in the abdomen. The picture may show a tumor or blocked ducts.
- EUS: Your doctor passes a thin, lighted tube (endoscope) down your throat, through your stomach, and into the first part of the small intestine. An ultrasound probe at the end of the tube sends out sound waves that you can’t hear. The waves bounce off tissues in your pancreas and other organs. As your doctor slowly withdraws the probe from the intestine toward the stomach, the computer creates a picture of the pancreas from the echoes. The picture can show a tumor in the pancreas. It can also show how deeply the cancer has invaded the blood vessels.
Some doctors use the following tests also:
- ERCP: The doctor passes an endoscope through your mouth and stomach, down into the first part of your small intestine. Your doctor slips a smaller tube through the endoscope into the bile ducts and pancreatic ducts. (See picture of ducts.) After injecting dye through the smaller tube into the ducts, the doctor takes x-ray pictures. The x-rays can show whether the ducts are narrowed or blocked by a tumor or other condition.
- MRI: A large machine with a strong magnet linked to a computer is used to make detailed pictures of areas inside your body.
- PET scan: You’ll receive an injection of a small amount of radioactive sugar. The radioactive sugar gives off signals that the PET scanner picks up. The PET scanner makes a picture of the places in your body where the sugar is being taken up. Cancer cells show up brighter in the picture because they take up sugar faster than normal cells do. A PET scan may show a tumor in the pancreas. It can also show cancer that has spread to other parts of the body.
- Needle biopsy: The doctor uses a thin needle to remove a small sample of tissue from the pancreas. EUS or CT may be used to guide the needle. A pathologist uses a microscope to look for cancer cells in the tissue.
If cancer of the pancreas is diagnosed, your doctor needs to learn the extent (stage) of the disease to help you choose the best treatment.
Pancreatic Cancer
There are two main types of pancreatic cancer.
Most often, pancreatic cancer starts in the ducts that carry pancreatic juices. This type is called exocrine pancreatic cancer. Information will focus on this type of pancreatic cancer.
Much less often, pancreatic cancer begins in the cells that make hormones. This type may be called endocrine pancreatic cancer or islet cell cancer.
Each year in the United States, more than 43,000 people are diagnosed with cancer of the pancreas. Most are over 65 years old. Visit the National Cancer Institute where this information and more can be found about Pancreatic Cancer or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el cáncer de páncreas en español.
Oral Cancer Treatment Options
People with early oral cancer may be treated with surgery or radiation therapy. People with advanced oral cancer may have a combination of treatments. For example, radiation therapy and chemotherapy are often given at the same time. Another treatment option is targeted therapy.
The choice of treatment depends mainly on your general health, where in your mouth or throat the cancer began, the size of the tumor, and whether the cancer has spread.
Surgery
Surgery to remove the tumor in the mouth or throat is a common treatment for oral cancer. Sometimes the surgeon also removes lymph nodes in the neck. Other tissues in the mouth and neck may be removed as well. You may have surgery alone or in combination with radiation therapy.
Also, surgery may cause tissues in your face to swell. This swelling usually goes away within a few weeks. However, removing lymph nodes can result in swelling that lasts a long time.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It’s an option for small tumors or for people who can’t have surgery. Or, it may be used before surgery to shrink the tumor. It also may be used after surgery to destroy cancer cells that may remain in the area.
Doctors use two types of radiation therapy to treat oral cancer. Some people with oral cancer have both types:
- External radiation therapy: The radiation comes from a machine. Some treatment centers offer IMRT, which uses a computer to more closely target the oral tumor to lessen the damage to healthy tissue. You may go to the hospital or clinic once or twice a day, generally 5 days a week for several weeks. Each treatment takes only a few minutes.
- Internal radiation therapy (implant radiation therapy or brachytherapy): Internal radiation therapy isn’t commonly used for oral cancer. The radiation comes from radioactive material in seeds, wires, or tubes put directly in the mouth or throat tissue. You may need to stay in the hospital for several days. Usually the radioactive material is removed before you go home.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. The drugs that treat oral cancer are usually given through a vein (intravenous). The drugs enter the bloodstream and travel throughout your body. Chemotherapy and radiation therapy are often given at the same time.
Targeted Therapy
Some people with oral cancer receive a type of drug known as targeted therapy. It may be given along with radiation therapy or chemotherapy.
Cetuximab (Erbitux) was the first targeted therapy approved for oral cancer. Cetuximab binds to oral cancer cells and interferes with cancer cell growth and the spread of cancer. You may receive cetuximab through a vein once a week for several weeks at the clinic.
Oral Cancer Staging
If oral cancer is diagnosed, your doctor needs to learn the extent (stage) of the disease to help you choose the best treatment. When oral cancer spreads, cancer cells may be found in the lymph nodes in the neck or in other tissues of the neck. Cancer cells can also spread to the lungs, liver, bones, and other parts of the body.
When cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells as the primary (original) tumor. For example, if oral cancer spreads to the lungs, the cancer cells in the lungs are actually oral cancer cells. The disease is called metastatic oral cancer, not lung cancer. It’s treated as oral cancer, not lung cancer. Doctors sometimes call the new tumor “distant” or metastatic disease.
Your doctor may order one or more of the following tests:
- X-rays: An x-ray of your entire mouth can show whether cancer has spread to the jaw. Images of your chest and lungs can show whether cancer has spread to these areas.
- CT scan: An x-ray machine linked to a computer takes a series of detailed pictures of your body. You may receive an injection of dye. Tumors in your mouth, throat, neck, lungs, or elsewhere in the body can show up on the CT scan.
- MRI: A powerful magnet linked to a computer is used to make detailed pictures of your body. An MRI can show whether oral cancer has spread.
- Endoscopy: The doctor uses a thin, lighted tube (endoscope) to check your throat, windpipe, and lungs. The doctor inserts the endoscope through your nose or mouth. Local anesthesia is used to ease your discomfort and prevent you from gagging. Some people also may be given a mild sedative. Sometimes the doctor uses general anesthesia to put a person to sleep. This exam may be done in a doctor’s office, an outpatient clinic, or a hospital.
- PET scan: You receive an injection of a small amount of radioactive sugar. The radioactive sugar gives off signals that the PET scanner picks up. The PET scanner makes a picture of the places in your body where the sugar is being taken up. Cancer cells show up brighter in the picture because they take up sugar faster than normal cells do. A PET scan shows whether oral cancer may have spread.
Doctors describe the stage of oral cancer based on the size of the tumor, whether it has invaded nearby tissues, and whether it has spread to the lymph nodes or other tissues:
- Early cancer: Stage I or II oral cancer is usually a small tumor (smaller than a walnut), and no cancer cells are found in the lymph nodes.
- Advanced cancer: Stage III or IV oral cancer is usually a large tumor (as big as a lime). The cancer may have invaded nearby tissues or spread to lymph nodes or other parts of the body.
Oral Cancer Diagnosis
If you have symptoms that suggest oral cancer, your doctor or dentist will check your mouth and throat for red or white patches, lumps, swelling, or other problems. A physical exam includes looking carefully at the roof of your mouth, back of your throat, and insides of your cheeks and lips. The floor of your mouth and lymph nodes in your neck will also be checked.
An ear, nose, and throat specialist can see the back of your nose, tongue, and throat by using a small, long-handled mirror or a lighted tube. Sometimes pictures need to be made with a CT scan or MRI to find a hidden tumor. (The Staging section describes imaging tests.)
The removal of a small piece of tissue to look for cancer cells is called a biopsy. Usually, a biopsy is done with local anesthesia. Sometimes, it’s done under general anesthesia. A pathologist then looks at the tissue under a microscope to check for cancer cells. A biopsy is the only sure way to know if the abnormal area is cancer.
Oral Cancer
Cancer that forms in tissues of the oral cavity (the mouth) or the oropharynx (the part of the throat at the back of the mouth).
This includes areas under the tongue
- Lips
- Gums and teeth
- Tongue
- Lining of your cheeks
- Salivary glands (glands that make saliva)
- Floor of your mouth (area under the tongue
This includes areas of the throat
- Roof of your mouth (hard palate)
- Soft palate
- Uvula
- Oropharynx
- Tonsils
Visit the National Cancer Institute where this information and more can be found about Oral Cancer or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el cáncer oral en español.
Kidney Cancer Treatment Options
Common treatment options for people with kidney cancer are surgery, targeted therapy, and biological therapy. You may receive more than one type of treatment.
The treatment that’s right for you depends mainly on the following:
- The size of the tumor
- Whether the tumor has invaded tissues outside the kidney
- Whether the tumor has spread to other parts of the body
- Your age and general health
Surgery
Surgery is the most common treatment for people with kidney cancer. The type of surgery depends on the size and stage of the cancer, whether you have two kidneys, and whether cancer was found in both kidneys.
You and your surgeon can talk about the types of surgery and which may be right for you:
- Removing all of the kidney (radical nephrectomy): The surgeon removes the entire kidney along with the adrenal gland and some tissue around the kidney. Some lymph nodes in the area may also be removed.
- Removing part of the kidney (partial nephrectomy): The surgeon removes only the part of the kidney that contains the tumor. People with a kidney tumor that is smaller than a tennis ball may choose this type of surgery.
There are two approaches for removing the kidney. The surgeon may remove the tumor by making a large incision into your body (open surgery). Or the surgeon may remove the tumor by making small incisions (laparoscopic surgery). The surgeon sees inside your abdomen with a thin, lighted tube (a laparoscope) placed inside a small incision.
The surgeon may use other methods of destroying the cancer in the kidney. For people who have a tumor smaller than 4 centimeters and who can’t have surgery to remove part of the kidney because of other health problems, the surgeon may suggest:
- Cryosurgery: The surgeon inserts a tool through a small incision or directly through the skin into the tumor. The tool freezes and kills the kidney tumor.
- Radiofrequency ablation: The surgeon inserts a special probe directly through the skin or through a small incision into the tumor. The probe contains tiny electrodes that kill the kidney cancer cells with heat.
Targeted Therapy
People with kidney cancer that has spread may receive a type of drug called targeted therapy. Many kinds of targeted therapy are used for kidney cancer. This treatment may shrink a kidney tumor or slow its growth.Usually, the targeted therapy is taken by mouth. You may want to read the NCI fact sheet Targeted Cancer Therapies.
Biological Therapy
People with kidney cancer that has spread may receive biological therapy. Biological therapy for kidney cancer is a treatment that may improve the body’s natural defense (the immune system response) against cancer. The treatments used for kidney cancer can slow the growth of tumors or shrink them. The biological therapy is injected intravenously or under the skin. The treatment may be given at the hospital or a doctor’s office.
Kidney Cancer Staging
If kidney cancer is diagnosed, your doctor needs to learn the extent (stage) of the disease to help you choose the best treatment. The stage is based on the size of the kidney tumor and whether the cancer has invaded nearby tissues or spread to other parts of the body.
Your doctor may order one or more tests:
- Blood tests: Your doctor can check for substances in your blood. Some people with kidney cancer have high levels of calcium or LDH. A blood test can also show how well your liver is working.
- Chest x-ray: An x-ray of the chest can show a tumor in your lung.
- CT scan: CT scans of your chest and abdomen can show cancer in your lymph nodes, lungs, or elsewhere.
- MRI: MRI can show cancer in your blood vessels, lymph nodes, or other tissues in the abdomen.
When cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary (original) tumor. For example, if kidney cancer spreads to a lung, the cancer cells in the lung are actually kidney cancer cells. The disease is metastatic kidney cancer, not lung cancer. It’s treated as kidney cancer, not as lung cancer.
These are the stages of kidney cancer:
- Stage I: The tumor is no bigger than a tennis ball (almost 3 inches or about 7 centimeters). Cancer cells are found only in the kidney.
- Stage II: The tumor is bigger than a tennis ball. But cancer cells are found only in the kidney.
- Stage III: The tumor can be any size. It has spread to at least one nearby lymph node. Or it has grown through the kidney to reach nearby blood vessels.
- Stage IV: The tumor has grown through the layer of fatty tissue and the outer layer of fibrous tissue that surrounds the kidney. Or cancer cells have spread to nearby lymph nodes or to the lungs, liver, bones, or other tissues.
Kidney Cancer Diagnosis
If you have symptoms that suggest kidney cancer, your doctor will try to find out what’s causing the problems.
You may have a physical exam. Also, you may have one or more of the following tests:
- Urine tests: The lab checks your urine for blood and other signs of disease.
- Blood tests: The lab checks your blood for several substances, such as creatinine. A high level of creatinine may mean the kidneys aren’t doing their job.
- Ultrasound: An ultrasound device uses sound waves that can’t be heard by humans. The sound waves make a pattern of echoes as they bounce off organs inside your abdomen. The echoes create a picture of your kidney and nearby tissues. The picture can show a kidney tumor.
- CT scan: An x-ray machine linked to a computer takes a series of detailed pictures of your abdomen. You may receive an injection of contrast material so your urinary tract and lymph nodes show up clearly in the pictures. The CT scan can show cancer in the kidneys, lymph nodes, or elsewhere in the abdomen.
- MRI: A large machine with a strong magnet linked to a computer is used to make detailed pictures of your urinary tract and lymph nodes. You may receive an injection of contrast material. MRI can show cancer in your kidneys, lymph nodes, or other tissues in the abdomen.
- IVP: You’ll receive an injection of dye into a vein in your arm. The dye travels through the body and collects in your kidneys. The dye makes them show up on x-rays. A series of x-rays then tracks the dye as it moves through your kidneys to your ureters and bladder. The x-rays can show a kidney tumor or other problems. (IVP is not used as commonly as CT or MRI for the detection of kidney cancer.)
- Biopsy: The removal of tissue to look for cancer cells is a biopsy. In some cases, your doctor will do a biopsy to diagnose kidney cancer. Your doctor inserts a thin needle through your skin into the kidney to remove a small sample of tissue. Your doctor may use ultrasound or a CT scan to guide the needle. A pathologist uses a microscope to check for cancer cells in the tissue.
- Surgery: After surgery to remove part or all of a kidney tumor, a pathologist can make the final diagnosis by checking the tissue under a microscope for cancer cells.
Kidney Cancer
Kidney cancer is a cancer that forms in tissues of the kidneys. Kidney cancer includes renal cell carcinoma (cancer that forms in the lining of very small tubes in the kidney that filter the blood and remove waste products) and renal pelvis carcinoma (cancer that forms in the center of the kidney where urine collects). It also includes Wilms tumor, which is a type of kidney cancer that usually develops in children under the age of 5.
Visit the National Cancer Institute where this information and more can be found about Kidney Cancer or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el cáncer de riñón en español.
Endometrial Cancer Treatment Options
Treatment options for people with uterine cancer are surgery, radiation therapy, chemotherapy, and hormone therapy. You may receive more than one type of treatment.
Surgery
Surgery is the most common treatment for women with uterine cancer. You and your surgeon can talk about the types of surgery (hysterectomy) and which may be right for you.
The surgeon usually removes the uterus, cervix, and nearby tissues. The nearby tissues may include:
- Ovaries
- Fallopian tubes
- Nearby lymph nodes
- Part of the vagina
Surgery to remove lymph nodes may cause lymphedema (swelling) in one or both legs. Your health care team can tell you how to prevent or relieve lymphedema.
Radiation Therapy
Radiation therapy is an option for women with all stages of uterine cancer. It may be used before or after surgery. For women who can’t have surgery for other medical reasons, radiation therapy may be used instead to destroy cancer cells in the uterus. Women with cancer that invades tissue beyond the uterus may have radiation therapy and chemotherapy.
Radiation therapy uses high-energy rays to kill cancer cells. It affects cells in the treated area only.
Doctors use two types of radiation therapy to treat uterine cancer. Some women receive both types:
- External radiation therapy: A large machine directs radiation at your pelvis or other areas with cancer. The treatment is usually given in a hospital or clinic. You may receive external radiation 5 days a week for several weeks. Each session takes only a few minutes.
- Internal radiation therapy(also called brachytherapy): A narrow cylinder is placed inside your vagina, and a radioactive substance is loaded into the cylinder. This common method of brachytherapy may be repeated two or more times over several weeks. Once the radioactive substance is removed, no radioactivity is left in the body.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It may be used after surgery to treat uterine cancer that has an increased risk of returning after treatment. For example, uterine cancer that is a high grade or is Stage II, III, or IV may be more likely to return. Also, chemotherapy may be given to women whose uterine cancer can’t be completely removed by surgery. For advanced cancer, it may be used alone or with radiation therapy.
Chemotherapy for uterine cancer is usually given by vein (intravenous). It’s usually given in cycles. Each cycle has a treatment period followed by a rest period.
Hormone Therapy
Some uterine tumors need hormones to grow. These tumors have hormone receptors for the hormones estrogen, progesterone, or both. If lab tests show that the tumor in your uterus has these receptors, then hormone therapy may be an option.
Hormone therapy may be used for women with advanced uterine cancer. Also, some women with Stage I uterine cancer who want to get pregnant and have children choose hormone therapy instead of surgery.The most common drug used for hormone therapy is progesterone tablets.
Endometrial Cancer Diagnosis
If you have symptoms that suggest uterine cancer, your doctor will try to find out what’s causing the problems. You may have a physical exam and blood tests. Also, you may have one or more of the following tests:
- Pelvic exam: Your doctor can check your uterus, vagina, and nearby tissues for any lumps or changes in shape or size.
- Ultrasound: An ultrasound device uses sound waves that can’t be heard by humans. The sound waves make a pattern of echoes as they bounce off organs inside the pelvis. The echoes create a picture of your uterus and nearby tissues. The picture can show a uterine tumor. For a better view of the uterus, the device may be inserted into the vagina (transvaginal ultrasound).
- Biopsy: The removal of tissue to look for cancer cells is a biopsy. A thin tube is inserted through the vagina into your uterus. Your doctor uses gentle scraping and suction to remove samples of tissue. A pathologist examines the tissue under a microscope to check for cancer cells. In most cases, a biopsy is the only sure way to tell whether cancer is present.
Grade
If cancer is found, the pathologist studies tissue samples from the uterus under a microscope to learn the grade of the tumor. The grade tells how much the tumor tissue differs from normal uterine tissue. It may suggest how fast the tumor is likely to grow. Tumors with higher grades tend to grow faster than those with lower grades. Tumors with higher grades are also more likely to spread. Doctors use tumor grade along with other factors to suggest treatment options.
Endometrial Cancer Staging
If uterine cancer is diagnosed, your doctor needs to learn the extent (stage) of the disease to help you choose the best treatment. The stage is based on whether the cancer has invaded nearby tissues or spread to other parts of the body.
When cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary (original) tumor. For example, if uterine cancer spreads to the lung, the cancer cells in the lung are actually uterine cancer cells. The disease is metastatic uterine cancer, not lung cancer. It’s treated as uterine cancer, not as lung cancer. Doctors sometimes call the new tumor “distant” disease.
To learn whether uterine cancer has spread, your doctor may order one or more tests:
- Lab tests: A Pap test can show whether cancer cells have spread to the cervix, and blood tests can show how well the liver and kidneys are working. Also, your doctor may order a blood test for a substance known as CA-125. Cancer may cause a high level of CA-125.
- Chest x-ray: An x-ray of the chest can show a tumor in the lung.
- CT scan: An x-ray machine linked to a computer takes a series of detailed pictures of your pelvis, abdomen, or chest.
- MRI: A large machine with a strong magnet linked to a computer is used to make detailed pictures of your uterus and lymph nodes.
In most cases, surgery is needed to learn the stage of uterine cancer. The surgeon removes the uterus and may take tissue samples from the pelvis and abdomen. After the uterus is removed, it is checked to see how deeply the tumor has grown. Also, the other tissue samples are checked for cancer cells.
These are the stages of uterine cancer:
- Stage 0: The abnormal cells are found only on the surface of the inner lining of the uterus. The doctor may call this carcinoma in situ.
- Stage I: The tumor has grown through the inner lining of the uterus to the endometrium. It may have invaded the myometrium.
- Stage II: The tumor has invaded the cervix.
- Stage III: The tumor has grown through the uterus to reach nearby tissues, such as the vagina or a lymph node.
- Stage IV: The tumor has invaded the bladder or intestine. Or, cancer cells have spread to parts of the body far away from the uterus, such as the liver, lungs, or bones.
Endometrial Cancer
Endometrial cancer is a cancer that forms in the tissue lining the uterus (the small, hollow, pear-shaped organ in a woman’s pelvis in which a fetus develops). Most endometrial cancers are adenocarcinomas (cancers that begin in cells that make and release mucus and other fluids).
Visit the National Cancer Institute where this information and more can be found about Endometrial Cancer including side effects of treatments, support information and more. Or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el cáncer de endometrio en español.
Preventing Cancer
Factors That are Known to Increase the Risk of Cancer
Cigarette Smoking and Tobacco Use
Tobacco use is strongly linked to an increased risk for many kinds of cancer. Smoking cigarettes is the leading cause of the following types of cancer:
- Acute myelogenous leukemia (AML)
- Bladder cancer
- Cervical cancer
- Esophageal cancer
- Kidney cancer
- Lung cancer
- Oral cavity cancer
- Pancreatic cancer
- Stomach cancer
Not smoking or quitting smoking lowers the risk of getting cancer and dying from cancer. Scientists believe that cigarette smoking causes about 30% of all cancer deaths in the United States.
See the following National Cancer Institute PDQ summaries for more information:
Infections
Certain viruses and bacteria may be able to cause cancer. Viruses and other infection-causing agents cause more cases of cancer in the developing world (about 1 in 4 cases of cancer) than in developed nations (less than 1 in 10 cases of cancer). Examples of cancer-causing viruses and bacteria include:
- Human papillomavirus (HPV) increases the risk for cancers of the cervix, penis, vagina, anus, and oropharynx.
- Hepatitis B and hepatitis C viruses increase the risk for liver cancer.
- Epstein-Barr virus increases the risk for Burkitt lymphoma.
- Helicobacter pylori increases the risk for gastric cancer.
Two vaccines prevent infection by cancer-causing agents have already been developed and approved by the U.S. Food and Drug Administration (FDA). One is a vaccine to prevent infection with hepatitis B virus. The other protects against infection with strains of human papillomavirus (HPV) that cause cervical cancer. Scientists continue to work on vaccines against infections that cause cancer.
See the following National Cancer Institute PDQ summaries for more information:
- Cervical Cancer Prevention
- Liver (Hepatocellular) Cancer Prevention
- Stomach (Gastric) Cancer Prevention
- Oral Cancer Prevention
Radiation
Being exposed to radiation is a known cause of cancer. There are two main types of radiation linked with an increased risk for cancer:
- Ultraviolet radiation from sunlight: This is the main cause of nonmelanoma skin cancers.
- Ionizing radiation from medical x-rays and radon gas in our homes: Scientists believe that ionizing radiation causes leukemia, thyroid cancer, and breast cancer in women. Ionizing radiation may also be linked to myeloma and cancers of the lung, stomach, colon, esophagus, bladder, and ovary. Being exposed to radiation from diagnostic x-rays increases the risk of cancer in patients and x-ray technicians.
See the following National Cancer Institute PDQ summaries for more information:
Factors That May Affect the Risk of Cancer
Diet
The foods that you eat on a regular basis make up your diet. Diet is being studied as a risk factor for cancer. It is hard to study the effects of diet on cancer because a person’s diet includes foods that may protect against cancer and foods that may increase the risk of cancer.
It is also hard for people who take part in the studies to keep track of what they eat over a long period of time. This may explain why studies have different results about how diet affects the risk of cancer.
Some studies show that fruits and nonstarchy vegetables may protect against cancers of the mouth, esophagus, and stomach. Fruits may also protect against lung cancer.
Some studies have shown that a diet high in fat, proteins, calories, and red meat increases the risk of colorectal cancer, but other studies have not shown this.
It is not known if a diet low in fat and high in fiber, fruits, and vegetables lowers the risk of colorectal cancer. See the American Institute for Cancer Research for more information about foods that prevent cancer.
See the following PDQ summaries for more information:
Alcohol
Studies have shown that drinking alcohol is linked to an increased risk of the following types of cancers:
- Oral cancer
- Esophageal cancer
- Breast cancer
- Colorectal cancer (in men)
Drinking alcohol may also increase the risk of liver cancer and female colorectal cancer.
See the following National Cancer Institute PDQ summaries for more information:
- Breast Cancer Prevention
- Colorectal Cancer Prevention
- Esophageal Cancer Prevention
- Oral Cancer Prevention
- Liver (Hepatocellular) Cancer Prevention
Physical Activity
Studies show that people who are physically active have a lower risk of certain cancers than those who are not. It is not known if physical activity itself is the reason for this.
Studies show a strong link between physical activity and a lower risk of colorectal cancer. Some studies show that physical activity protects against postmenopausal breast cancer and endometrial cancer.
See the following National Cancer Institute PDQ summaries for more information:
Obesity
Studies show that obesity is linked to a higher risk of the following types of cancer:
- Postmenopausal breast cancer
- Colorectal cancer
- Endometrial cancer
- Esophageal cancer
- Kidney cancer
- Pancreatic cancer
Some studies show that obesity is also a risk factor for cancer of the gallbladder.
Studies do not show that losing weight lowers the risk of cancers that have been linked to obesity.
See the following National Cancer Institute PDQ summaries for more information:
- Breast Cancer Prevention
- Colorectal Cancer Prevention
- Endometrial Cancer Prevention
- Lung Cancer Prevention
Information provided the National Cancer Institute.
Adult Treatment Plans
What is Cancer?
Although there are many kinds of cancer, they all start because of out-of-control growth of abnormal cells. Normal body cells grow, divide, and die in an orderly fashion. Because cancer cells continue to grow and divide, they are different from normal cells. Instead of dying, they outlive normal cells and continue to form new abnormal cells.
When this abnormal cell growth occurs, the result can be the development of a lump, mass or tumor, which can be benign (non-cancerous) or malignant (cancerous). Cancer cells develop because of damage to DNA, which directs all activities in each cell. When DNA becomes damaged, the body is usually able to repair it. In cancer cells, however, the damaged DNA is not repaired.
Cancer comes in many forms, and the specific disease is named for the part of the body in which it begins. Cells from cancerous tumors can spread, or metastasize, throughout the body. For example, cancer that begins in the prostate but has spread to the bones is called metastatic prostate cancer. Some cancers involving the blood and blood-forming organs (bone marrow) do not form tumors, but circulate through other tissues where they grow.
Cancer Information
Knowledge is power when you’re dealing with cancer.
Today, millions of people are living with cancer or have had cancer. Florida Cancer Affiliates offers this extensive disease and drug information section with the intent of helping you learn more about cancer, and what you can expect for the "typical treatment" of common types of cancer.
Use this information to help you better understand the disease and make informed and timely choices for your treatment. Then speak with your Florida Cancer Affiliate physician about how a customized treatment plan will be developed to meet your specific care needs.
Our expert physicians and clinical staff are ready to help you, your family and caretakers through every step of this cancer journey.
Morton Grove
Thank You
Site Map
Privacy Policy
Terms of Use
Blog
Contact Us
Appointments
We know that patients facing cancer need rapid answers and the best treatment plans. To schedule your appointment, please call (352) 732-4032 and ask for the location that is nearest you.
Questions
For questions or inquiries related to your physician, appointments, prescriptions, PET scans, lab work, or to speak to your nurse, please call the specific physician office that you visit. .
Employment
Please fax resumes and employment inquiries to the HR Coordinators at 727.484.7782.
About The US Oncology Network
Florida Cancer Affiliates is a practice in The US Oncology Network (The Network). This collaboration unites the practice with more than 1,200 independent physicians dedicated to delivering value-based, integrated care to patients — close to home. Through The Network, these independent doctors come together to form a community of shared expertise and resources dedicated to advancing local cancer care and to delivering better patient outcomes. The Network is supported by McKesson Corporation, whose coordinated resources and infrastructure allow doctors in The Network to focus on the health of their patients, while McKesson focuses on the health of their practices. Florida Cancer Affiliates also participates in clinical trials through US Oncology Research, which has played a role in more than 100 FDA-approved cancer therapies, approximately one-third of all cancer therapies approved by the FDA to date. For more information, visit usoncology.com
Locations
To make an appointment, please call
1 (855) 451-7095
New Port Richey
5500 Little Road
New Port Richey, FL
34655
Tel 727.372.9159
Fax 727.376.8703
Spring Hill
11373 Cortez Boulevard # Suite 200
Brooksville, FL
34613
Tel 352.597.4998
Fax 352.596.6051
Physician Publications
Medical News on Cancer
Patient Forms
What You Need for an Appointment
Patients who fill out their patient forms, prior to their initial visit are more at ease during their appointment. It also saves you valuable time while you’re in our office.
To fill out your New Patient forms, click on the link below, print the form, and fill out as many fields as possible. Bring the forms with you to your first visit. Please take your time when filling out the forms, and provide as much information as you can about your complete health history.
Click here for the FCA Patient History Form.
Click here for the FCA HIPAA From.
Click here for the FCA Assignment of Benefits form.
Helpful Resources
While a person experiences a variety of emotions, when a person first learns that he/she has cancer or a blood disorder/disease, the primary concern is survival. As treatment begins, however, new issues become important. Some of these include relationships with others, side effects from treatments, and nutrition and diet. Living with cancer or a blood disease/disorder is challenging, and it is best to be educated about issues surrounding survival in order to live a full and productive life.
Below are links to websites containing information for people living with cancer or a blood disorder/disease. The content provided through these links is not the information of Cancer Care Centers of South Texas nor does the practice necessarily endorse such content. In addition, all content provided through these links is for information only and does not constitute medical advice. Please consult your physician before acting or relying upon such information.
National Organizations
American Cancer Society (ACS)
English
Espanol
American College of Radiation Oncology (ACRO)
www.acro.org
American Institute of Cancer Resarch
American Medical Association (AMA)
www.ama-assn.org
American Society of Hematology (ASH)
www.hematology.org
American Society for Therapeutic Radiology and Oncology (ASTRO)
www.astro.org
American Society of Clinical Oncology (ASCO)
www.asco.org
Association of Cancer Online Resources (ACOR)
www.acor.org
CancerEducation.com
www.cancereducation.com
Cancer News on the Net®
www.cancernews.com
Cancer Research Institute (CRI)
www.cancerresearch.org
Cancer.net
www.cancer.net
CancerGuide
www.cancerguide.org
Healthfinder
www.healthfinder.gov
Medline Plus
www.nlm.nih.gov/medlineplus
Myelodysplastic Syndromes Foundation
National Alliance for Caregiving (NAC)
www.caring.org
National Cancer Institute (NCI)
English
Espanol
National Comprehensive Cancer Network (NCCN)
www.nccn.org
Needy Meds
www.needymeds.com
National Institutes of Health (NIH)
www.nih.gov
National Library of Medicine (NLM)
www.nlm.nih.gov
OncoLink (University of Pennsylvania)
www.oncolink.org
Oncology Nursing Society (ONS)
www.ons.org
Planet Cancer
www.planetcancer.org
Quackwatch
www.quackwatch.com
Society of Gynecologic Oncologists
www.sgo.org
U.S. Food and Drug Administration (FDA)
www.fda.gov
US Oncology
www.usoncology.com
Disease-Specific Organizations
National Brain Tumor Society
www.braintumor.org
BreastCancer.org
www.breastcancer.org
Breast Cancer Network of Strength
(formerly Y-ME National Breast Cancer Organization)
www.networkofstrength.org
Colon Cancer Alliance
www.ccalliance.org
Leukemia & Lymphoma Society
www.leukemia-lymphoma.org
Lung Cancer Alliance
www.lungcanceralliance.org
Lymphoma Research Foundation
www.lymphoma.org
Ovarian Cancer National Alliance
www.ovariancancer.org
National Ovarian Cancer Coalition
www.ovarian.org
Prostate Cancer Foundation
www.pcf.org
Skin Cancer Foundation
www.skincancer.org
Local Organizations
Alamo Breast Cancer Foundation
www.alamobreastcancer.org
Alamo City Cancer Council
www.alamocitycancercouncil.org
Leukemia/Lymphoma Society South Texas Chapter
www.leukemia-lymphoma.org/all_chap
Susan G. Komen San Antonio Chapter
www.komensanantonio.org
Patient Advocacy/Survivorship
National Coalition for Cancer Survivorship
www.canceradvocacy.org
Cancer Survivors Network
csn.cancer.org
National Cancer Survivor Day® Foundation, Inc.
www.ncsdf.org
National Patient Advocate Foundation (NPAF)
www.npaf.org
Patient Advocate Foundation
www.patientadvocate.org
Patient & Family Support Services
Caring Connections
www.caringinfo.org
Gilda’s Club Worldwide
www.gildasclub.org
Lance Armstrong Foundation
www.livestrong.org
Life Beyond Cancer Foundation
www.lifebeyondcancer.org
Look Good…Feel Better
English
Espanol
National Center for Complementary and Alternative Medicine
www.nccam.nih.gov
National Family Caregivers Association (NFCA)
www.nfcacares.org
People Living Through Cancer
www.pltc.org
US TOO Prostate Cancer Support Group
www.ustoo.com
The Wellness Community
www.thewellnesscommunity.org
Personalized Treatment Plan
Treatment Options
People with multiple myeloma have many treatment options. The options are watchful waiting, induction therapy, and stem cell transplant. Sometimes a combination of methods is used.
Radiation therapy is used sometimes to treat painful bone disease. It may be used alone or along with other therapies. See the Supportive Care section to learn about ways to relieve pain.
The choice of treatment depends mainly on how advanced the disease is and whether you have symptoms. If you have multiple myeloma without symptoms (smoldering myeloma), you may not need cancer treatment right away. The doctor monitors your health closely (watchful waiting) so that treatment can start when you begin to have symptoms.
If you have symptoms, you will likely get induction therapy. Sometimes a stem cell transplant is part of the treatment plan.
When treatment for myeloma is needed, it can often control the disease and its symptoms. People may receive therapy to help keep the cancer in remission, but myeloma can seldom be cured. Because standard treatment may not control myeloma, you may want to talk to your doctor about taking part in a clinical trial. Clinical trials are research studies of new treatment methods.
Watchful Waiting
People with smoldering myeloma or Stage I myeloma may be able to put off having cancer treatment. By delaying treatment, you can avoid the side effects of treatment until you have symptoms.
If you and your doctor agree that watchful waiting is a good idea, you will have regular checkups (such as every 3 months). You will receive treatment if symptoms occur.
Although watchful waiting avoids or delays the side effects of cancer treatment, this choice has risks. In some cases, it may reduce the chance to control myeloma before it gets worse.
You may decide against watchful waiting if you don’t want to live with untreated myeloma. If you choose watchful waiting but grow concerned later, you should discuss your feelings with your doctor. Another approach is an option in most cases.
Induction Therapy
Many different types of drugs are used to treat myeloma. People often receive a combination of drugs, and many different combinations are used to treat myeloma.
Each type of drug kills cancer cells in a different way:
- Chemotherapy: Chemotherapy kills fast-growing myeloma cells, but the drug can also harm normal cells that divide rapidly.
- Targeted therapy: Targeted therapies use drugs that block the growth of myeloma cells. The targeted therapy blocks the action of an abnormal protein that stimulates the growth of myeloma cells.
- Steroids: Some steroids have antitumor effects. It is thought that steroids can trigger the death of myeloma cells. A steroid may be used alone or with other drugs to treat myeloma.
You may receive the drugs by mouth or through a vein (IV). The treatment usually takes place in an outpatient part of the hospital, at your doctor’s office, or at home. Some people may need to stay in the hospital for treatment.
Stem Cell Transplant
Many people with multiple myeloma may get a stem cell transplant. A stem cell transplant allows you to be treated with high doses of drugs. The high doses destroy both myeloma cells and normal blood cells in the bone marrow. After you receive high-dose treatment, you receive healthy stem cells through a vein. (It’s like getting a blood transfusion.) New blood cells develop from the transplanted stem cells. The new blood cells replace the ones that were destroyed by treatment.
Stem cell transplants take place in the hospital. Some people with myeloma have two or more transplants.
Stem cells may come from you or from someone who donates their stem cells to you:
- From you: An autologous stem cell transplant uses your own stem cells. Before you get the high-dose chemotherapy, your stem cells are removed. The cells may be treated to kill any myeloma cells present. Your stem cells are frozen and stored. After you receive high-dose chemotherapy, the stored stem cells are thawed and returned to you.
- From a family member or other donor: An allogeneic stem cell transplant uses healthy stem cells from a donor. Your brother, sister, or parent may be the donor. Sometimes the stem cells come from a donor who isn’t related. Doctors use blood tests to be sure the donor’s cells match your cells. Allogeneic stem cell transplants are under study for the treatment of multiple myeloma.
- From your identical twin: If you have an identical twin, a syngeneic stem cell transplant uses stem cells from your healthy twin.
There are two ways to get stem cells for people with myeloma. They usually come from the blood (peripheral blood stem cell transplant). Or they can come from the bone marrow (bone marrow transplant).
After a stem cell transplant, you may stay in the hospital for several weeks or months. You’ll be at risk for infections because of the large doses of chemotherapy you received. In time, the transplanted stem cells will begin to produce healthy blood cells.
Staging
If the biopsy shows that you have multiple myeloma, your doctor needs to learn the extent (stage) of the disease to plan the best treatment. Staging may involve having more tests:
- Blood tests: For staging, the doctor considers the results of blood tests, including albumin and beta-2-microglobulin.
- CT scan: An x-ray machine linked to a computer takes a series of detailed pictures of your bones.
- MRI: A powerful magnet linked to a computer is used to make detailed pictures of your bones.
Doctors may describe multiple myeloma as
- Smoldering
- Stage I
- Stage II
- Stage III
The stage takes into account whether the cancer is causing problems with your bones or kidneys. Smoldering multiple myeloma is early disease without any symptoms. For example, there is no bone damage. Early disease with symptoms (such as bone damage) is Stage I. Stage II or III is more advanced, and more myeloma cells are found in the body.
Diagnosis
Doctors sometimes find multiple myeloma after a routine blood test. More often, doctors suspect multiple myeloma after an x-ray for a broken bone. Usually though, patients go to the doctor because they are having other symptoms.
To find out whether such problems are from multiple myeloma or some other condition, your doctor may ask about your personal and family medical history and do a physical exam. Your doctor also may order some of the following tests:
-
Blood tests: The lab does several blood tests:
- Multiple myeloma causes high levels of proteins in the blood. The lab checks the levels of many different proteins, including M protein and other immunoglobulins (antibodies), albumin, and beta-2-microglobulin.
- Myeloma may also cause anemia and low levels of white blood cells and platelets. The lab does a complete blood count to check the number of white blood cells, red blood cells, and platelets.
- The lab also checks for high levels of calcium.
- To see how well the kidneys are working, the lab tests for creatinine.
- Urine tests: The lab checks for Bence Jones protein, a type of M protein, in urine. The lab measures the amount of Bence Jones protein in urine collected over a 24-hour period. If the lab finds a high level of Bence Jones protein in your urine sample, doctors will monitor your kidneys. Bence Jones protein can clog the kidneys and damage them.
- X-rays: You may have x-rays to check for broken or thinning bones.An x-ray of your whole body can be done to see how many bones could be damaged by the myeloma.
- Biopsy: Your doctor removes tissue to look for cancer cells. A biopsy is the only sure way to know whether myeloma cells are in your bone marrow. Before the sample is taken, local anesthesia is used to numb the area. This helps reduce the pain. Your doctor removes some bone marrow from your hip bone or another large bone. A pathologist uses a microscope to check the tissue for myeloma cells.
There are two ways your doctor can obtain bone marrow. Some people will have both procedures during the same visit:
- Bone marrow aspiration: The doctor uses a thick, hollow needle to remove samples of bone marrow.
- Bone marrow biopsy: The doctor uses a very thick, hollow needle to remove a small piece of bone and bone marrow.
Multiple Myeloma
Myeloma begins when a plasma cell becomes abnormal. The abnormal cell divides to make copies of itself. The new cells divide again and again, making more and more abnormal cells. These abnormal plasma cells are called myeloma cells.
In time, myeloma cells collect in the bone marrow. They may damage the solid part of the bone. When myeloma cells collect in several of your bones, the disease is called “multiple myeloma.” This disease may also harm other tissues and organs, such as the kidneys.
Myeloma cells make antibodies called M proteins and other proteins. These proteins can collect in the blood, urine, and organs.
Visit the National Cancer Institute where this information and more can be found about Multiple Myeloma or ask your cancer care team questions about your individual situation.
Treatment Options
Your doctor can describe your treatment choices and the expected results. You and your doctor can work together to develop a treatment plan that meets your needs.
Your doctor may refer you to a specialist, or you may ask for a referral. Specialists who treat Hodgkin lymphoma include hematologists, medical oncologists, and radiation oncologists . Your doctor may suggest that you choose an oncologist who specializes in the treatment of Hodgkin lymphoma. Often, such doctors are associated with major academic centers. Your health care team may also include an oncology nurse and a registered dietitian.
The choice of treatment depends mainly on the following:
- The type of your Hodgkin lymphoma (most people have classical Hodgkin lymphoma)
- Its stage (where the lymphoma is found)
- Whether you have a tumor that is more than 4 inches (10 centimeters) wide
- Your age
- Whether you’ve had weight loss, drenching night sweats, or fevers.
People with Hodgkin lymphoma may be treated with chemotherapy, radiation therapy, or both.
If Hodgkin lymphoma comes back after treatment, doctors call this a relapse or recurrence. People with Hodgkin lymphoma that comes back after treatment may receive high doses of chemotherapy, radiation therapy, or both, followed by stem cell transplantation.
Chemotherapy
Chemotherapy for Hodgkin lymphoma uses drugs to kill lymphoma cells. It is called systemic therapy because the drugs travel through the bloodstream. The drugs can reach lymphoma cells in almost all parts of the body.
Usually, more than one drug is given. Most drugs for Hodgkin lymphoma are given through a vein (intravenous), but some are taken by mouth.
Chemotherapy is given in cycles. You have a treatment period followed by a rest period. The length of the rest period and the number of treatment cycles depend on the stage of your disease and on the anticancer drugs used.
You may have your treatment in a clinic, at the doctor’s office, or at home. Some people may need to stay in the hospital for treatment.
Radiation Therapy
Radiation therapy (also called radiotherapy) for Hodgkin lymphoma uses high-energy rays to kill lymphoma cells. It can shrink tumors and help control pain.
A large machine aims the rays at the lymph node areas affected by lymphoma. This is local therapy because it affects cells in the treated area only. Most people go to a hospital or clinic for treatment 5 days a week for several weeks.
Stem Cell Transplantation
If Hodgkin lymphoma returns after treatment, you may receive stem cell transplantation. A transplant of your own blood-forming stem cells (autologous stem cell transplantation) allows you to receive high doses of chemotherapy, radiation therapy, or both. The high doses destroy both Hodgkin lymphoma cells and healthy blood cells in the bone marrow.
Stem cell transplants take place in the hospital. Before you receive high-dose treatment, your stem cells are removed and may be treated to kill lymphoma cells that may be present. Your stem cells are frozen and stored. After you receive high-dose treatment to kill Hodgkin lymphoma cells, your stored stem cells are thawed and given back to you through a flexible tube placed in a large vein in your neck or chest area. New blood cells develop from the transplanted stem cells.
Staging
The doctor considers the following to determine the stage of Hodgkin lymphoma:
- The number of lymph nodes that have Hodgkin lymphoma cells
- Whether these lymph nodes are on one or both sides of the diaphragm (see picture)
- Whether the disease has spread to the bone marrow, spleen, liver, or lung.
The stages of Hodgkin lymphoma are as follows:
- Stage I: The lymphoma cells are in one lymph node group (such as in the neck or underarm). Or, if the lymphoma cells are not in the lymph nodes, they are in only one part of a tissue or an organ
- Stage II: The lymphoma cells are in at least two lymph node groups on the same side of (either above or below) the diaphragm. Or, the lymphoma cells are in one part of a tissue or an organ and the lymph nodes near that organ (on the same side of the diaphragm). There may be lymphoma cells in other lymph node groups on the same side of the diaphragm.
- Stage III: The lymphoma cells are in lymph nodes above and below the diaphragm. Lymphoma also may be found in one part of a tissue or an organ (such as the liver, lung, or bone) near these lymph node groups. It may also be found in the spleen.
- Stage IV: Lymphoma cells are found in several parts of one or more organs or tissues. Or, the lymphoma is in an organ (such as the liver, lung, or bone) and in distant lymph nodes.
- Recurrent: The disease returns after treatment.
In addition to these stage numbers, your doctor may also describe the stage as A or B:
- A: You have not had weight loss, drenching night sweats, or fevers.
- B: You have had weight loss, drenching night sweats, or fevers.
Diagnosis
If you have swollen lymph nodes or another symptom that suggests Hodgkin lymphoma, your doctor will try to find out what’s causing the problem. Your doctor may ask about your personal and family medical history.
You may have some of the following exams and tests:
- Physical exam: Your doctor checks for swollen lymph nodes in your neck, underarms, and groin. Your doctor also checks for a swollen spleen or liver.
- Blood tests: The lab does a complete blood count to check the number of white blood cells and other cells and substances.
- Chest x-rays: X-ray pictures may show swollen lymph nodes or other signs of disease in your chest.
- Biopsy: A biopsy is the only sure way to diagnose Hodgkin lymphoma. Your doctor may remove an entire lymph node (excisional biopsy) or only part of a lymph node (incisional biopsy). A thin needle (fine needle aspiration) usually cannot remove a large enough sample for the pathologist to diagnose Hodgkin lymphoma. Removing an entire lymph node is best.
The pathologist uses a microscope to check the tissue for Hodgkin lymphoma cells. A person with Hodgkin lymphoma usually has large, abnormal cells known as Reed-Sternberg cells. They are not found in people with non-Hodgkin lymphoma. See the photo of a Reed-Sternberg cell.
Hodgkin Lymphoma
Hodgkin lymphoma is a cancer that begins in cells of the immune system. The immune system fights infections and other diseases.
Hodgkin lymphoma can start almost anywhere. Usually, it's first found in a lymph node above the diaphragm, the thin muscle that separates the chest from the abdomen. But Hodgkin lymphoma also may be found in a group of lymph nodes. Sometimes it starts in other parts of the lymphatic system.
Hodgkin Lymphoma Cells
Hodgkin lymphoma begins when a lymphocyte (usually a B cell) becomes abnormal. The abnormal cell is called a Reed-Sternberg cell. (See photo below.)
The Reed-Sternberg cell divides to make copies of itself. The new cells divide again and again, making more and more abnormal cells. The abnormal cells don't die when they should. They don't protect the body from infections or other diseases. The buildup of extra cells often forms a mass of tissue called a growth or tumor.
Visit the National Cancer Institute where this information and more can be found about Hodgkin Lymphoma or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el linfoma de Hodgkin.
Regions: Northern Florida | Central Florida
Specialties
Medical Oncology
Hematology
Specialties
Medical Oncology
Hematology
Specialties
Medical Oncology
Hematology
Radiation Oncology