Due to recent changes in Federal healthcare regulations, telehealth services are no longer being covered under the temporary policies that were put in place during the COVID-19 pandemic. As coverage reverts to pre-pandemic standards, we regret to inform you that our clinic will no longer offer telehealth appointments effective 10/01/2025.
In February, our practice was impacted by the national outage experienced by Change Healthcare because of a cyberattack. Change Healthcare is a healthcare technology company, part of Optum and United Healthcare, that provides services used by much of the US healthcare system, including our practice.
We have remained in close contact with Change Healthcare as they investigate and address this issue.
Change Healthcare has begun issuing customer notifications related to the February 2024 cyberattack. On April 22, 2024, Change Healthcare publicly confirmed the impacted data could cover a substantial proportion of people in America. More recently, on June 20, 2024, Change Healthcare notified our practice’s management company that some of its data was compromised.
At this time, Florida Cancer Affiliates has not been notified of any specific patients of the practice whose protected health information has been affected by the incident.
For more information, please visit https://www.changehealthcare.com/hipaa-substitute-notice.
If you are looking to refill a medication dispensed by Florida Cancer Affiliates in Ocala, please fill out the form below. If you have questions about your prescription refill, call us at (352)547-1915.
For all other prescriptions not filled by us, please contact your pharmacy directly.
The health and safety of our patients is our top priority. We are closely monitoring COVID-19, including the latest updates from the Centers for Disease Control and Prevention (CDC). The CDC-recommended protocols for healthcare providers regarding COVID-19 are aligned with our existing protocols for flu season. During flu season, we emphasize an array of preventative measures that protect our patients and staff from exposure to illness.
In addition to our existing protocols and our rigorous cleaning procedures, to further ensure the safety of those we serve, we have:
Prior authorization, grant, and copay assistance experts.
Working hand-in-hand with your physicians and prescribers.
Prescription refill reminders and ready reminders.
Accepting many forms of payment and most insurances.
Open Monday to Friday, 8:30am to 5pm, or 24 hours via call center.
Refill prescriptions from Florida Cancer Affiliates here.
For more information, call (352)547-1915 or email us at FCAPharmacy@usoncology.com, or visit us in person at 3130 SW 32nd Ave, Ocala, FL 34474.
See our Medication Refill Policy.
 Ocala, Fl, Florida Cancer Affiliates proudly announces it has achieved accreditation through the Accreditation Commission for Health Care (ACHC) for the services of Specialty Pharmacy.
Ocala, Fl, Florida Cancer Affiliates proudly announces it has achieved accreditation through the Accreditation Commission for Health Care (ACHC) for the services of Specialty Pharmacy.
Accreditation is a process through which healthcare organizations demonstrate compliance with national standards. Accreditation by ACHC reflects an organization’s dedication and commitment to meeting standards that facilitate a higher level of performance and patient care.
ACHC is a nonprofit organization that has stood as a symbol of quality and excellence since 1986. ACHC is ISO 9001:2015 certified and has CMS deeming authority for Home Health, Hospice, and DMEPOS.
Florida Cancer Affiliates is committed to providing patients with the specialized care they need, along with the tools, resources, and personal support that will help them navigate through their journey with cancer. We offer our patients the latest technology and therapies, ranging from leading-edge diagnostic imaging to sophisticated forms of radiation therapy. At the same time, we are dedicated to delivering your care with the compassion you desire. Our patients have access to the best therapies and current treatment options, including clinical trials, right here in our own community.
This specialty accreditation means that Florida Cancer Affiliates can bring more specialized pharmaceutical care to patients without having to rely on outside pharmacies to deliver their oral medications.
Make the best choice for your cancer care. Call for an appointment today.
For more information, call (352)547-1915.
Florida Cancer Affiliates will continue to provide excellent care for your hematology and oncology needs if you so choose. Patients have the opportunity to reschedule their appointments with physicians in our group, with no records transfer and no headaches. All your information is already in our shared database
The doctors below are listed in order of availability. Please click on the doctor’s name to see physician bio. Our staff will be ready to assist you in transferring your care.
|
850-769-2996 |
850-769-2996 |
850-763-0036 |
850-215-5300 |
850-763-0036 |
|
2614 Jenks Avenue |
2614 Jenks Avenue |
2100 State Avenue |
2417 Jenks Avenue |
2100 State Avenue |
You may also want to contact your referring provider for their preference. Medical records will continue to be held by Florida Cancer Affiliates, and available upon request as always.
Dear Patient
It has been a pleasure to treat patients with cancer and blood disorders for the past 34 years. I have had the privilege serving members of our beautiful community for over 10 years, and have developed lifelong friendships with many of my patients. It’s been an honor to be entrusted with your care.
After lots of soul searching and consulting with my family and friends, I have made a decision to announce my retirement from hematology oncology, effective February 29th, 2016. Over the past three decades, I have cherished the memories I shared with my patients. Working with cancer patients has been a gratifying and rewarding experience for me. I wouldn’t trade that time for anything. I hope you will accept my retirement for what it is: a cherished reward for a lifetime of hard work. I’m ready and excited to begin the next phase in my life.
As I go towards my new adventure, Florida Cancer Affiliates will continue to provide excellent care for your hematology and oncology needs. Patients will have the opportunity to reschedule their appointments with physicians in our group. The doctors above are listed in order of availability. Our staff will ready to assist you in transferring your care. You may also want to contact your referring provider for their preference. I have made arrangements to be available to my partners during this transition phase, and you can be confident you will continue to receive the compassionate and innovative care you’re accustomed to. I have utmost confidence and respect for the doctors in my group. You will be in great hands.
Medical records will continue to be held by Florida Cancer Affiliates, and available upon request as always.
Thank you again for allowing me to serve you as your physician. It has been an honor.
Most sincerely,
John Nanfro, M.D., F.A.C.P.
Thank you for submitting your electronic payment.
For questions or comments please contact: .(JavaScript must be enabled to view this email address)
You may contact us by calling 1-800-998-3450 and a representative will be happy to help you.
Thank you for choosing Florida Cancer Affiliates.
There are several convenient options for you to make a payment.
Florida Cancer Affiliates
PO BOX 946205
Atlanta, GA 30394-6205
Call with questions about your bill: (800) 630‑4670; Monday – Friday, 8:30AM – 4:30PM (Eastern)
 A Randomized Phase 3 Study of Sitravatinib in Combination With Nivolumab Versus Docetaxel in Patients With Advanced Non-Squamous Non-Small Cell Lung Cancer With Disease Progression On or After Platinum-Based Chemotherapy and Checkpoint Inhibitor Therapy (SAPPHIRE)
A Randomized Phase 3 Study of Sitravatinib in Combination With Nivolumab Versus Docetaxel in Patients With Advanced Non-Squamous Non-Small Cell Lung Cancer With Disease Progression On or After Platinum-Based Chemotherapy and Checkpoint Inhibitor Therapy (SAPPHIRE)
https://clinicaltrials.gov/ct2/show/NCT03906071
Double Blinded, Placebo-Controlled Phase III Study to Evaluate the Efficacy and Safety of Canakinumab Vs Placebo as Adjuvant Therapy in Adult Subjects with Stages II-IIIA and IIIB (T>5cm N2) Completely Resected (R0) Non-Small Cell Lung Cancer (NSCLC)
https://www.clinicaltrials.gov/ct2/show/NCT03447769#contacts
A Phase 2 Randomized, Multicenter, Double-Blind Study of the Glutaminase Inhibitor Telaglenastat with Pembrolizumab and Chemotherapy Versus Placebo with Pembrolizumab and Chemotherapy in First-Line, Metastatic KEAP1/NRF2-Mutated, Nonsquamous, Non-Small Cell Lung Cancer (NSCLC)
https://clinicaltrials.gov/ct2/show/NCT04265534
Study of JNJ-61186372, a Human Bispecific EGFR and cMet Antibody, in Participants With Advanced Non-Small Cell Lung Cancer - Drugs: JNJ-61186372, Lazertinib, Pemetrexed, Carboplatin, JNJ-61186372 - EGFR and MET
https://clinicaltrials.gov/ct2/show/NCT02609776
 A Phase III, Multicenter, Randomized, Double-blind, Placebo-controlled Study to Assess the Efficacy and Safety of Alpelisib (BYL719) in Combination With Nab-paclitaxel in Patients With Advanced Triple Negative Breast Cancer With Either Phosphoinositide-3-kinase Catalytic Subunit Alpha (PIK3CA) Mutation or Phosphatase and Tensin Homolog Protein (PTEN) Loss Without PIK3CA Mutation
A Phase III, Multicenter, Randomized, Double-blind, Placebo-controlled Study to Assess the Efficacy and Safety of Alpelisib (BYL719) in Combination With Nab-paclitaxel in Patients With Advanced Triple Negative Breast Cancer With Either Phosphoinositide-3-kinase Catalytic Subunit Alpha (PIK3CA) Mutation or Phosphatase and Tensin Homolog Protein (PTEN) Loss Without PIK3CA Mutation
https://www.clinicaltrials.gov/ct2/show/NCT04251533
Evaluation of Lasofoxifene Versus Fulvestrant in Advanced or Metastatic ER+/HER2− Breast Cancer With an ESR1 Mutation - Drugs: Lasofoxifene, Fulvestrant - ESR1 mutations
https://clinicaltrials.gov/ct2/show/NCT03781063
Evaluation of Lasofoxifene Combined With Abemaciclib in Advanced or Metastatic ER+/HER2− Breast Cancer With an ESR1 Mutation - Drugs: Lasofoxifene and abemaciclib (VERZENIO).- ESR1 mutations
https://clinicaltrials.gov/ct2/show/NCT04432454
 Phase I/II Study of the Safety, Pharmacokinetics, and Preliminary Clinical Activity of BT8009 in Patients with Nectin-4 Expressing Advanced Malignancies
Phase I/II Study of the Safety, Pharmacokinetics, and Preliminary Clinical Activity of BT8009 in Patients with Nectin-4 Expressing Advanced Malignancies
https://clinicaltrials.gov/ct2/show/NCT04561362?term=BT8009-100&draw=2&rank=1
Phase 1/1b Study to Evaluate the Safety and Activity of TTX-030 (Anti-CD39) in Combination with Budigalimab (Anti-PD-1) and/or mFOLFOX6 in Subjects with Solid Tumors
https://clinicaltrials.gov/ct2/show/NCT04306900
A First-in-human, Phase 1 Study to Evaluate the Safety of TTX-080, an HLA-G Antagonist, in Subjects with Advanced Solid Tumors
https://clinicaltrials.gov/ct2/show/NCT04485013
A phase 1/2 study of IDE196 in patients with solid tumors harboring GNAQ/11 mutations or PRKC fusions Drugs: IDE196 - GNAQ or GNA11 mutations or PRKC fusions
https://clinicaltrials.gov/ct2/show/NCT03947385
A Phase 1/2 Multiple Expansion Cohort Trial of MRTX849 in Patients with Advanced Solid Tumors with KRAS G12C Mutation - Drugs: MRTX849, Pembrolizumab, Cetuximab, Afatinib - KRAS G12C
https://clinicaltrials.gov/ct2/show/NCT03785249 Mutation
A Phase 2 Study of Seribantumab in Adult Patients with Neuregulin-1 (NRG1) Fusion Positive Locally Advanced or Metastatic Solid Tumors - Drugs: Seribantumab - Neuregulin-1 (NRG1) Fusion
https://www.clinicaltrials.gov/ct2/show/NCT04383210
A Phase I/II Study of MCLA-128, a full length IgG1 Bispecific Antibody Targeting HER2 and HER3, in Patients with Solid Tumors - Drugs: zenocutuzumab (MCLA-128) - Neuregulin-1 (NRG1) Fusion
https://clinicaltrials.gov/ct2/show/NCT02912949
A Phase 1/2 Multicenter Study of the Safety, Pharmacokinetics, and Preliminary Efficacy of APL-101 in Subjects with Non-Small Cell Lung Cancer with c-Met EXON 14 Skip Mutations and c-Met Dysregulation Advanced Solid Tumors - Drugs: APL-101 Oral Capsules - c-Met EXON 14 Skip Mutations c-Met Dysregulation
https://www.clinicaltrials.gov/ct2/show/NCT03175224
A Phase 2 Study of Seribantumab in Adult Patients With NRG1 Gene Fusion Positive Cancer - Drugs: Seribantumab - NRG1 Fusion
https://clinicaltrials.gov/ct2/show/NCT04383210
A Study of Erdafitinib in Participants With Advanced Solid Tumors and Fibroblast Growth Factor Receptor (FGFR) Gene Alterations - FGFR
https://clinicaltrials.gov/ct2/show/NCT04083976
A Study of Repotrectinib (TPX-0005) in Patients With Advanced Solid Tumors Harboring ALK, ROS1, or NTRK1-3 Rearrangements - Drugs: Oral repotrectinib (TPX-0005) - ROS1, or NTRK1-3 Rearrangements
https://clinicaltrials.gov/ct2/show/NCT03093116
PK,PD, Safety and Tolerability of Multiple Dose Regimens of MT-3724 With Lenalidomide for the Treatment of Patients With Relapsed/Refractory Diffuse Large B Cell Non-Hodgkin's Lymphoma (MT-3724_NHL_003) - Drugs: MT-3724 - CD20
https://clinicaltrials.gov/ct2/show/NCT03645395
PK,PD, Safety and Tolerability of Multiple Dose Regimens of MT-3724 With Gemcitabine and Oxaliplatin for the Treatment of Patients With Relapsed/Refractory Diffuse Large B Cell Non-Hodgkin's Lymphoma - Drugs: MT-3724 - CD20
https://clinicaltrials.gov/ct2/show/NCT03488251
A Randomized Phase 3 Study to Evaluate the Efficacy and Safety of Enzastaurin Plus R-CHOP Versus R-CHOP in Treatment-Naïve Subjects with High-Risk Diffuse Large B-Cell Lymphoma Who Possess the Novel Genomic Biomarker DGM1™ - Drugs: Enzastaurin (Kinenza®), R-CHOP, Placebo - Positive for Genomic Biomarker DGM1
https://clinicaltrials.gov/ct2/show/NCT03263026
Open-label, Active-controlled, Multicenter Phase II Study to Investigate the Efficacy and Safety of UV1 Vaccination in Combination with Nivolumab and Ipilimumab as First-line Treatment of Patients with Unresectable or Metastatic Melanoma (UV1-202)
https://clinicaltrials.gov/ct2/show/NCT04382664
A Study of Niraparib in Combination With Abiraterone Acetate and Prednisone Versus Abiraterone Acetate and Prednisone for Treatment of Participants With Metastatic Prostate Cancer - Drugs: Niraparib, Abiraterone Acetate, Prednisone, Placebo - BRCA 1/2 and CDK12
https://clinicaltrials.gov/ct2/show/NCT03748641
A Phase 2/3 Trial to Evaluate Margetuximab in Combination with Chemotherapy and CPI or Trastuzumab and Chemotherapy alone in Patients with Treatment-naïve Metastatic or Locally Advanced, Her2-positive Gastric or Gastroesophageal Junction Cancer
https://clinicaltrials.gov/ct2/show/NCT04082364
A Phase 2 Study of the Hepcidin Mimetic PTG-300 in Patients with Phlebotomy-Requiring Polycythemia Vera
https://clinicaltrials.gov/ct2/show/NCT04057040
A Phase 3, Multicenter, Randomized, Double-Blinded, Placebo-Controlled Trial to Evaluate the Efficacy and Safety of Efgartigimod (ARGX-113) 10 mg/kg IV in Adult Patients with ITP
https://clinicaltrials.gov/ct2/show/NCT04188379
A Randomized, Dose-ranging, Open-label, Parallel Group Study to Assess the Efficacy, Safety and Pharmacokinetics of Palonosetron HCl Buccal Film versus IV Palonosetron 0.25 mg (ALOXI®) for the Prevention of Chemotherapy-induced Nausea and Vomiting in Cancer Patients Receiving Moderately Emetogenic Chemotherapy
https://www.clinicaltrials.gov/ct2/show/NCT04592198
We have access to over 30 trials through Tempus’ and Caris PharmaTech’s Just-in-Time activation program. These trials can be activated within 2 weeks of identifying an eligible sub
Over the past 40 years, Ocala Oncology/Florida Cancer Affiliates has provided our patients access to cutting-edge and innovative clinical trials in a comfortable and convenient setting. One of the largest and most reputable community-based research networks in the world, US Oncology Research has contributed to over 70 FDA-approved cancer therapies and approximately one-third of all FDA-approved oncology therapies. It also specializes in Phase I–IV oncology clinical trials and has participated in over 1,600 investigator-initiated and sponsor-initiated trials since its inception. The program brings innovative therapies and clinical trials to practices and patients in communities across the nation to help advance the science of cancer care while offering the best possible treatments and improved patient outcomes.
We are proud of our new role in the research and development of vital new cancer therapies through independent studies. This will alow us broader range of opportunities to offer our patients . We are dedicated to advancing cancer care by leading and participating in clinical trials that test the safety and efficiency of new or modified treatments. And we are deeply committed to bringing clinical trials to our community, offering patients an opportunity to help shape the future of cancer treatment, while benefitting from the very latest in clinical trials. Ocala Oncology/Florida Cancer Affiliates is constantly offering eligible patients opportunities to join new trials.
At Ocala Oncology/Florida Cancer Affiliates,research is an integral part of our comprehensive efforts to provide cancer patients in our community with access to the latest and most advanced therapies and treatment options. We now have access to Sarah Cannon Research Trials.
We are pleased to share this list of clinical trials currently enrolling at our practice.
I am pleased to share an update regarding our progress with the MYLUNG Consortium™ research study in metastatic non-small cell lung cancer (mNSCLC). Results from the first phase were released during the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting by The US Oncology Network (The Network), US Oncology Research and Ontada™.
Makenzi Evangelist, MD, physician lead for the study and oncologist with New York Oncology Hematology, presented the findings during an oral presentation at ASCO titled, “Biomarker tissue journey among patients with untreated metastatic non-small cell lung cancer (mNSCLC) in The US Oncology Network community practices.” (ASCO Abstract 9004)
Protocol 1 (out of 3) provides a retrospective look at chart data and allows us to draw early conclusions about historical baseline trends for testing patterns and identify gaps in the data that need to be filled with the prospective research the MYLUNG Consortium will address in the next protocol.
Protocol 1 findings include:
Data from Protocol 1 will be compared to Protocol 2, which will prospectively evaluate contemporary ordering patterns and turnaround times. It will enroll about 1,000 patients from 11 sites across The Network and will monitor the real-world patient journey from presentation through their first line of cancer therapy, focusing on how diagnostic biomarker information is obtained, utilized and operationalized in decision-making. Patients are currently being enrolled in this stage of the study.
In addition to recognizing the progress that’s been made through this innovative research, I want to acknowledge the growing number of consortium participants and welcome two new life science companies. Genentech and AstraZeneca have joined this collaborative effort along with current members Amgen, Eli Lilly and Company and Mirati Therapeutics.
We will continue to grow the MYLUNG Consortium to reach up to 7,500 patients from approximately 20 Network sites over a five-year period during Protocol 3, integrating findings from the previous protocols and exploring new processes and associated outcomes. Thank you to the participating physicians and patients – together we are enabling providers to make the best treatment recommendations while improving access to testing and therapies for patients with lung cancer.
For more information, visit the MYLUNG webpage and blog on usoncology.com
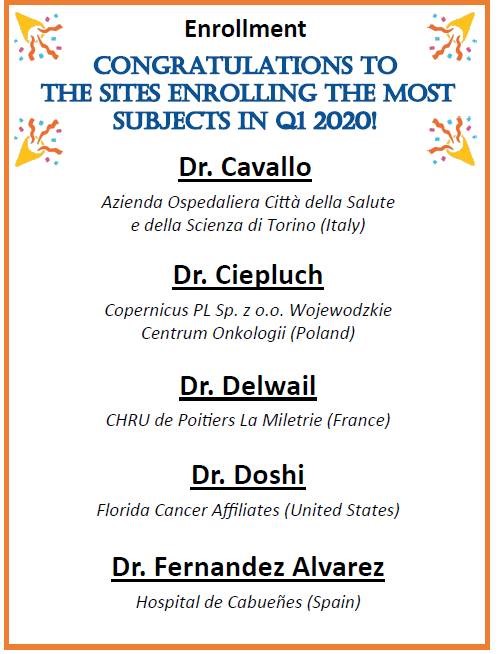
Congratulation to Dr. Ketan Doshi and the research team at Ocala Oncology/Florida Cancer Affiliates for being recognized as the top enrolling site in the United States for a Follicular Lymphoma study evaluating patients receiving the combination of Ibrutinib and Rituximab for the treatment of follicular lymphoma. View Clinical Trials
Different types of treatment are available for patients with melanoma. These are the five treatment options commonly used for melanoma depending on the stage of the cancer.
Surgery to remove the tumor is the primary treatment of all stages of melanoma. The doctor may remove the tumor as well as check to see if the cancer has spread to the lymph system.
Skin grafting (taking skin from another part of the body to replace the skin that is removed) may be done to cover the wound caused by surgery.
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body. This is called systemic chemotherapy.
When chemotherapy is placed directly into the spinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas. This is regional chemotherapy.
One type of regional chemotherapy used for melanoma patients is used to inject the anticancer drugs directly to the arm or leg the cancer is in. The flow of blood to and from the limb is temporarily stopped with a tourniquet. A warm solution with the anticancer drugs is put directly into the blood of the limb. This gives a high dose of drugs to the area where the cancer is.
The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Even if the doctor removes all the melanoma during surgery, there can be some left that can’t be seen. Some patients may be offered chemotherapy after surgery to kill any cancer cells that are left. Chemotherapy given after surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
Biologic therapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This type of cancer treatment is also called biotherapy or immunotherapy.
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. The following types of targeted therapy are being used in the treatment of melanoma:
body text
boody
Treatment for idiopathic thrombocytopenic purpura (ITP) is based on how much and how often you’re bleeding and your platelet count. In some cases, treatment may not be needed. Medicines often are used as the first course of treatment. Treatments used for children and adults are similar. Adults with ITP who have very low platelet counts or problems with bleeding often are treated. Adults who have milder cases of ITP may not need any treatment, other than watching their symptoms and platelet counts.
If adults or children who have ITP need treatment, medicines often are tried first. Corticosteroids, such as prednisone, are commonly used to treat ITP. These medicines, called steroids for short, help increase your platelet count by lowering the activity of your immune system. However, steroids have a number of side effects, and some people relapse (get worse) when treatment ends. The steroids used to treat ITP are different from illegal steroids taken by some athletes to enhance performance. Corticosteroids aren't habit-forming, even if you take them for many years.
Some medicines used to help raise the platelet count are given through a needle inserted into a vein. These medicines include immune globulin and anti-Rh (D) immunoglobulin.
Medicines also may be used along with a procedure to remove the spleen, called splenectomy. If steroids, immunoglobulins, or splenectomy don’t help, two newer medicines—eltrombopag and romiplostim—can be used to treat ITP.
If necessary, the spleen will be removed surgically. This organ is located in the upper left abdomen. The spleen is about the size of a golf ball in children and a baseball in adults. The spleen makes antibodies (proteins) that help fight infection. In ITP, these antibodies destroy platelets. If ITP hasn't responded to steroids, removing the spleen will reduce the destruction of platelets. However, it also may make you more likely to get certain infections. Before you have the surgery, your doctor may give you vaccines to help prevent these infections. If your spleen is removed, your doctor will explain what steps you can take to help avoid infections and what symptoms to watch for.
Some people with ITP who have severe bleeding may need to have platelet transfusions and be hospitalized. Some people will need a platelet transfusion before having surgery. For a platelet transfusion, donor platelets from a blood bank are injected into the recipient's bloodstream. This increases the platelet count for a short time.
There are two types of ITP: acute (temporary or short-term) and chronic (long-lasting).
People who have ITP often have purple bruises that appear on the skin or on the mucous membranes (for example, in the mouth). The bruises mean that bleeding has occurred in small blood vessels under the skin. A person who has ITP also may have bleeding that results in tiny red or purple dots on the skin. These pinpoint-sized dots are called petechiae. Petechiae may look like a rash. Bleeding under the skin causes the purple, brown, and red color of the petechiae and purpura.
People who have ITP also may have nosebleeds, bleeding from the gums when they have dental work done, or other bleeding that's hard to stop. Women who have ITP may have menstrual bleeding that's heavier than usual.
More extensive bleeding can cause hematomas. A hematoma is a collection of clotted or partially clotted blood under the skin. It looks or feels like a lump. Bleeding in the brain as a result of ITP is very rare, but can be life threatening if it occurs.
In most cases, an autoimmune response is believed to cause ITP. Normally your immune system helps your body fight off infections and diseases. But if you have ITP, your immune system attacks and destroys its own platelets. The reason why this happens isn’t known. ITP can't be passed from one person to another.
Treatment of essential thrombocythemia in patients younger than 60 years who have no symptoms and an acceptable platelet count is usually watchful waiting. Treatment of other patients may include the following:
Essential thrombocythemia often does not cause early symptoms. It is sometimes found during a routine blood test called the Complete Blood Count. The following symptoms may be caused by essential thrombocytopenia or by other conditions. A doctor should be consulted if any of these problems occur:
Platelets are sticky. When there are too many platelets, they may clump together and make it hard for the blood to flow. Clots may form in blood vessels and there may also be increased bleeding. These can cause serious health problems such as stroke or heart attack.
Treatment of primary myelofibrosis in patients without symptoms is usually watchful waiting. Treatment of primary myelofibrosis in patients with symptoms may include the following:
Possible signs of primary myelofibrosis include pain below the ribs on the left side and feeling very tired.
Primary myelofibrosis often does not cause early symptoms. It is sometimes found during a routine blood test. The following symptoms may be caused by primary myelofibrosis or by other conditions. A doctor should be consulted if any of these problems occur:
In addition to a complete blood count, bone marrow aspiration and biopsy, and cytogenetic analysis, a peripheral blood smear is used to diagnose primary myelofibrosis. A peripheral blood smear is a procedure in which a sample of blood is checked for tear drop-shaped red blood cells, the number and kinds of white blood cells, the number of platelets, and the presence of blast cells.
Treatment of de novo and secondary myelodysplastic syndromes may include the following:
Treatment of previously treated myelodysplastic syndromes may include the following:
There is no staging system for myelodysplastic syndromes. Treatment is based on whether the disease developed after the patient was exposed to factors that cause myelodysplastic syndrome or whether the disease was previously treated. Myelodysplastic syndromes are grouped for treatment as follows:
Tests that examine the blood and bone marrow are used to detect (find) and diagnose myelodysplastic syndromes. The following tests and procedures may be used:
Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
Complete blood count (CBC) with differential: A procedure in which a sample of blood is drawn and checked for the following:
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions.
Peripheral blood smear: A procedure in which a sample of blood is checked for changes in the number, type, shape, and size of blood cells and for too much iron in the red blood cells.
Cytogenetic analysis: A test in which cells in a sample of blood or bone marrow are viewed under a microscope to look for certain changes in the chromosomes.
Bone marrow aspiration and biopsy: The removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone. A pathologist views the bone marrow, blood, and bone under a microscope to look for abnormal cells.
Myelodysplastic syndromes are diagnosed based on certain changes in the blood cells and bone marrow.
There are several types of myelodysplastic syndromes.
Myelodysplastic syndromes have too few of one or more types of healthy blood cells in the bone marrow or blood. Myelodysplastic syndromes include the following diseases:
Our expert team of oncology and hematology specialists treat patients with a broad range of cancer types and hematological disorders including those listed below.
Adrenal Cortical Cancer
Anal Cancer
Aplastic Anemia
Bile Duct Cancer
Bladder Cancer
Bone Cancer
Bone Metastasis
Brain and Central Nervous System Tumors
Breast Cancer
Cervical Cancer
Coagulation Disorders
Colon and Rectal Cancer
Deep Vein Thrombosis
Endometrial Cancer
Eye Cancer
Follicular Lymphoma
Gallbladder Cancer
Gastrointestinal Tumors
Gestational Trophoblastic Disease
Hodgkin's Disease
Immune Thrombocytopenic Purpura
Kidney Cancer
Laryngeal and Hypopharyngeal Cancer
Leukemia
Liver Cancer
Lung Cancer
Male Breast Cancer
Malignant Mesothelioma
Multiple Myeloma
Myelodysplastic Syndrome
Nasal Cavity and Paranasal Cancer
Nasopharyngeal Cancer
Neuroblastoma
Non-Hodgkin’s Lymphoma
Oral Cavity and Oropharyngeal Cancer
Osteosarcoma
Ovarian Cancer
Pancreatic Cancer
Pituitary Tumor
Prostate Cancer
Retinoblastoma
Rhabdomyosarcoma
Salivary Gland Cancer
Sarcoma
Stomach Cancer
Testicular Cancer
Thrombocytopenia
Thymus Cancer
Thyroid Cancer
Studies have shown that support groups are very beneficial for the survival and quality of life for cancer patients, their families and caregivers. The following resources are available to cancer patients and their families in the Ocala area:
Located in the Florida Cancer Affiliates' Main Ocala office, this room offers patients an array of free products for their cancer journey, including wigs, blankets, hats, port covers, pillows and more. This is open to the public for anyone that has a need because of cancer. 433 SW 10th Street in Ocala.
This is a monthly meeting for breast cancer survivors to share their experience and be informed and educated on treatments and treatments available during their journey. This is offered the LAST Tuesday of each month at 1:00 pm at Ocala West United Church, 9330 SW 105th Street in Ocala. For more information, contact 352-291-6904.
The Cancer Alliance of Marion County offers quarterly educational programs to inform medical professions and patients of the many aspects of cancer care. There will be an opportunity to mingle as both patients and professionals share knowledge and insight together. Seating is limited and dinner is provided. For more information, contact 352-401-1534
Support group for all interested patients, care givers, family members and friends are encouraged to join. The Stomping Out Myeloma Support Group meets every second Saturday of each month at 11:00am at the Howard Academy, 306 NW 7th Avenue in Ocala. For more information, please contact 352-671-3060.
Share your cancer stories and bond with others going through the cancer journey. This cancer support group meets the 4th Friday of each month at 1:30 in the Advent Health Ocala Auxilliary Building. 1542 SW 1st Avenue, Ocala. Please contact Laura at 352-690-5675 for more information.
Particpants in these groups support each other, identify with one another, and gain some added strength from a relaxed comfortable group setting. During these meetings, participants are encouraged to vent their feelings and share their experiences, but coming to listen can often be helpful too. Participants continually experience many healing connections and positive experiences during this important time together.
When a person first learns that they have cancer or a blood disorder/disease the primary concern is survival. As treatment begins, however, new issues become more important. Some of these include relationships with others, side effects from treatments, and nutrition and diet.
Living with cancer or a blood disease/disorder is challenging, and it is best to be educated about issues surrounding survival in order to live a full and productive life.
Below are links to websites containing information for people living with cancer or a blood disorder/disease. The content provided through these links is not the information of Florida Cancer Affiliates, nor does the practice necessarily endorse the content. In addition, all content provided through these links is for information only and does not constitute medical advice. Please consult your Florida Cancer Affiliates physician before acting or relying upon such information.
American Cancer Society (ACS)
English
Espanol
American College of Radiation Oncology (ACRO)
http://www.acro.org
American Institute of Cancer Resarch
American Medical Association (AMA)
http://www.ama-assn.org
American Society of Hematology (ASH)
http://www.hematology.org
American Society for Therapeutic Radiology and Oncology (ASTRO)
http://www.astro.org
American Society of Clinical Oncology (ASCO)
http://www.asco.org
Association of Cancer Online Resources (ACOR)
http://www.acor.org
CancerEducation.com
http://www.cancereducation.com
Cancer News on the Net®
http://www.cancernews.com
Cancer Research Institute (CRI)
http://www.cancerresearch.org
Cancer.net
http://www.cancer.net
CancerGuide
http://www.cancerguide.org
Healthfinder
http://www.healthfinder.gov
Medline Plus
http://www.nlm.nih.gov/medlineplus
Myelodysplastic Syndromes Foundation
www.mds-foundation.org
National Alliance for Caregiving (NAC)
http://www.caring.org
National Cancer Institute (NCI)
English
Espanol
National Comprehensive Cancer Network (NCCN)
http://www.nccn.org
Needy Meds
http://www.needymeds.com
National Institutes of Health (NIH)
http://www.nih.gov
National Library of Medicine (NLM)
http://www.nlm.nih.gov
OncoLink (University of Pennsylvania)
http://www.oncolink.org
Oncology Nursing Society (ONS)
http://www.ons.org
Planet Cancer
http://www.planetcancer.org
Quackwatch
http://www.quackwatch.com
Society of Gynecologic Oncologists
http://www.sgo.org
U.S. Food and Drug Administration (FDA)
http://www.fda.gov
US Oncology
http://www.usoncology.com
National Brain Tumor Society
http://www.braintumor.org
BreastCancer.org
http://www.breastcancer.org
Breast Cancer Network of Strength
(formerly Y-ME National Breast Cancer Organization)
http://www.networkofstrength.org
Colon Cancer Alliance
http://www.ccalliance.org
Leukemia & Lymphoma Society
http://www.leukemia-lymphoma.org
Lung Cancer Alliance
http://www.lungcanceralliance.org
Lymphoma Research Foundation
http://www.lymphoma.org
The Mesothelioma Center
http://asbestos.com
Mesothelioma Guide
http://www.mesotheliomaguide.com/
Ovarian Cancer National Alliance
http://www.ovariancancer.org
National Ovarian Cancer Coalition
http://www.ovarian.org
Prostate Cancer Foundation
http://www.pcf.org
Skin Cancer Foundation
http://www.skincancer.org
National Coalition for Cancer Survivorship
http://www.canceradvocacy.org
Cancer Survivors Network
csn.cancer.org
National Cancer Survivor Day® Foundation, Inc.
http://www.ncsdf.org
National Patient Advocate Foundation (NPAF)
http://www.npaf.org
Patient Advocate Foundation
http://www.patientadvocate.org
Patient & Family Support Services
Caring Connections
http://www.caringinfo.org
Gilda’s Club Worldwide
http://www.gildasclub.org
Lance Armstrong Foundation
http://www.livestrong.org
Life Beyond Cancer Foundation
http://www.lifebeyondcancer.org
Look Good…Feel Better
English
Espanol
National Center for Complementary and Alternative Medicine
http://www.nccam.nih.gov
National Family Caregivers Association (NFCA)
http://www.nfcacares.org
People Living Through Cancer
http://www.pltc.org
US TOO Prostate Cancer Support Group
http://www.ustoo.com
The Wellness Community
http://www.thewellnesscommunity.org
Your Florida Cancer Affiliates physician may include PET and CT scans in your cancer care plan, as these tests can greatly improve our ability to evaluate and treat your disease. The PET and CT scan brings two powerful imaging techniques and combines them into one of the most advanced medical imaging tools available. It answers questions such as: where is the tumor, how big is it, is it malignant, benign or due to inflammatory change, and has it spread?
Positron Emission Tomography (PET) shows a body’s metabolic activity, while Computed Tomography (CT) shows anatomy. When fused together, the information from these two scans can be used with a high degree of confidence to detect, localize and assess the exact stage for a variety of cancers.
The scan reveals your body’s metabolic pattern, including both normal and abnormal tissue activity, such as a tumor. At the same time, the CT scan reveals the detailed anatomy of the area where the normal and abnormal activity is taking place. The improved images reduce the number of invasive procedures required during diagnosis and follow up care for most patients.
A PET scan alone is very helpful in showing the presence or spread of many malignant tumors. When it is combined with a CT scan in the same session, our physicians are able to pinpoint the exact location of a tumor, more accurately assess the stage of the disease and follow the progress of each patient’s treatments.
Screening exams can diagnose cancer at the earliest stages, when treatment will be the most effective. Florida Cancer Affiliates recommends that patients have routine screening and/or self-exams for breast, prostate, colorectal, skin, testicular and cervical cancers.
The screening guidelines below offer recommended timing for specific ages, genders, and cancer types.
At Florida Cancer Affiliates, we encourage and connect patients and their families with the best supportive services for all the educational, emotional and financial challenges they may be facing at this difficult time.
If you have cancer and are undergoing cancer treatment, there are places in our community that offer additional help. There are many local organizations throughout the country that offer a variety of practical support services to patients with cancer.
Many of the national cancer organizations, such as the American Cancer Society, can assist you in finding additional support services in your area.
Visit our Helpful Websites page for more information, or call our practice at any time and we will be glad to assist you.
Florida Cancer Affiliates has embraced clinical trial research as a critical component of community-based care for our patients with cancer or blood disorders. Participating in clinical trials shows us what works (and what doesn't) in medicine. Plus, they are the best way for our doctors to learn what is safe and effective in treating diseases such as cancer.
Clinical research offers us access to new investigational drugs (not always available to the general public); it reduces treatment-related side effects and introduces new methods of care for our patients.
We access clinical trials through our affiliation with The US Oncology Research Network, one of the nation's largest healthcare networks dedicated to cancer treatment and clinical trial research, specializing in Phase I-IV clinical trials. This affiliation allows us to provide patients in the communities that we serve, access to many of the most current and innovative clinical trials available. The US Oncology Research Network has contributed to the development of 39 anti-cancer drugs approved by the FDA.
If you would like more information, please ask your physician about available clinical trials that might be suitable for you.
Below is a list of questions that you might have when discussing clinical trials with your Ocala Oncology/Florida Cancer Affiliates physician. If you express an interest in a clinical trial, we will explain the research trial process, and address any questions you might have prior to starting any research procedures in a process known as Informed Consent.
The Informed Consent discussion should address many of the questions below, and is an opportunity for you to have your questions answered prior to deciding to participate in a clinical trial.
If you have any questions or need more information about your treatment or research studies currently in progress, please let us know.
For more information on clinical trials, visit The US Oncology Network Clinical Trials page or the National Cancer Institute.
Targeted cancer therapies interfere with cancer cell division and growth in many different ways. Some of these therapies focus on proteins that are involved in cell messaging pathways, which form a complicated communication process that directs basic cellular functions and activities, such as cell division, cell movement, how a cell responds to different outside stimuli, and even cell death.
Targeted cancer therapies block these bad signals that tell cancer cells to grow and divide uncontrollably. By doing this, the therapies can help stop cancer development and can cause cancer cell death through a process known as apoptosis.
Other targeted therapies can cause cancer cell death by actually making apoptosis happen. Sometimes it happens indirectly, by boosting a patient’s immune system to see and kill cancer cells, and bringing the deadly ingredients right to them.
To learn more and to see what types of cancer are currently being treated with targeted therapies, visit the National Cancer Institute.
Idiopathic thrombocytopenic purpura (ITP) is a bleeding condition in which the blood doesn't clot as it should. This is due to a low number of blood cell fragments called platelets. Platelets also are called thrombocytes which are made in your bone marrow along with other kinds of blood cells. Platelets stick together (clot) to seal small cuts or breaks on blood vessel walls and stop bleeding. "Idiopathic" means that the cause of the condition isn't known. "Thrombocytopenic" means there's a lower than normal number of platelets in the blood. "Purpura" refers to purple bruises caused by bleeding under the skin.
**All information about ITP is provided by the National Heart, Lung, and Blood Institute as a part of the National Institutes of Health and the U.S. Department of Health and Human Services
Cancer Care Centers of South Texas is affiliated with the Anticoagulation Clinics of North America (ACNA). ACNA is a complete anticoagulation and thrombosis management service providing high-quality, efficient care to patients receiving anticoagulation with warfarin (Coumadin) and antithrombotic medications (blood thinners and platelet inhibitors).
Services offered include both out-patient and in-hospital management of anticoagulant medications. In addition, ACNA offers a comprehensive out-patient treatment program for Deep Vein Thrombosis (DVT) and comprehensive evaluation and management of patients with thrombotic disorders. Most patients with deep vein thrombosis can now be evaluated and treated in our office without needing a hospital admission.
For extensive information about our anticoagulation and thrombosis management service, please see our complete website for the Anticoagulation Clinics of North America.
The bone marrow is made of tissues that make blood cells (red blood cells, white blood cells, and platelets) and a web of fibers that support the blood-forming tissues. In primary myelofibrosis (also called chronic idiopathic myelofibrosis), large numbers of blood stem cells develop into blood cells that do not mature properly (blasts). The web of fibers inside the bone marrow also becomes very thick (like scar tissue) and slows the blood-forming tissue’s ability to make blood cells. This causes the blood-forming tissues to make fewer and fewer blood cells. In order to make up for the low number of blood cells made in the bone marrow, the liver and spleen begin to make the blood cells.
Essential thrombocythemia is a disease in which too many platelets (thrombocytes) in the blood. This abnormal increase in the number of platelets in the blood is due to increased production by the bone marrow.
The purpose of treatment for polycythemia vera is to reduce the number of extra blood cells. Treatment of polycythemia vera may include the following:
A clinical trial of a new treatment.
The purpose of treatment for polycythemia vera is to reduce the number of extra blood cells. Treatment of polycythemia vera may include the following:
Possible signs of polycythemia vera include headaches and a feeling of fullness below the ribs on the left side.
Polycythemia vera often does not cause early symptoms. It is sometimes found during a routine blood test. Symptoms may occur as the number of blood cells increases. Other conditions may cause the same symptoms. A doctor should be consulted if any of the following problems occur:
Special blood tests are used to diagnose polycythemia vera. In addition to a complete blood count, bone marrow aspiration and biopsy, and cytogenetic analysis, a serum erythropoietin test is used to diagnose polycythemia vera. In this test, a sample of blood is checked for the level of erythropoietin (a hormone that stimulates new red blood cells to be made).
Polycythemia vera is a disease in which too many red blood cells are made in the bone marrow.
In polycythemia vera, the blood becomes thickened with too many red blood cells. The number of white blood cells and platelets may also increase. These extra blood cells may collect in the spleen and cause it to swell. The increased number of red blood cells or platelets in the blood can cause bleeding problems and make clots form in blood vessels. This can increase the risk of stroke or heart attack. In patients who are older than 65 years or who have a history of blood clots, the risk of stroke or heart attack is higher. Patients also have an increased risk of developing acute myeloid leukemia or primary myelofibrosis.
Myelodysplastic syndromes are a group of diseases in which the bone marrow does not make enough healthy blood cells.
Myelodysplastic syndromes are diseases of the blood and bone marrow. Normally, the bone marrow makes blood stem cells (immature cells) that develop into mature blood cells over time. A blood stem cell may become a myeloid stem cell or a lymphoid stem cell. The lymphoid stem cell develops into a white blood cell. The myeloid stem cell develops into one of three types of mature blood cells:
Cancer Care Centers of South Texas have been recognized nationally for expertise in the diagnosis, treatment and research of myelodysplasia and is designated as a "Center of Excellence" by the The Myelodysplastic Syndromes Foundation.
Lo que usted necesita saber sobre síndromes mielodisplásicos.
Need a presenter for a medical event?
Our physicians are available for speaking engagements.
Please use this guide for when you should call our office:
If your call is received after business hours (after 5 p.m.), or on weekends or holidays, the physician on call will be paged on your behalf and will respond quickly. Since your call may not be returned by your personal physician, please be prepared to provide the following information:
Please indicate in your phone message:
If you experience a life-threatening medical emergency, immediately call 911. Upon arrival at the emergency room, ask the staff to call your Florida Cancer Affiliates physician.
If you feel that you need immediate consultation, or advice regarding a serious condition, do not hesitate to call us at 1 (855) 451-7095 during regular business hours, Monday-Friday, 8:30am-5pm. Our clinical staff and physicians return patient calls during business hours between appointments and consultations. If your question is urgent, please tell our telephone operator, so that a provider or nurse can confer with you more promptly.
Please understand that calls for test results and prescription refills will be returned after urgent patient needs are met. All calls are returned in the order of medical priority.
Ocala Oncology/Florida Cancer Affiliates is a practice in The US Oncology Network (The Network). This collaboration unites the practice with more than 1,200 independent physicians dedicated to delivering value-based, integrated care to patients — close to home.
Through The Network, these independent doctors come together to form a community of shared expertise and resources dedicated to advancing local cancer care and to delivering better patient outcomes. The Network is supported by McKesson Corporation, whose coordinated resources and infrastructure allow doctors in The Network to focus on the health of their patients, while McKesson focuses on the health of their practices.
Ocala Oncology/Florida Cancer Affiliates also participates in clinical trials through US Oncology Research, which has played a role in more than 100 FDA-approved cancer therapies, approximately one-third of all cancer therapies approved by the FDA to date. For more information, visit usoncology.com
We appreciate that you are considering partnering with us on this very personal journey. As an important part of your care team, we commit to you:
Most patients diagnosed with early stage breast cancer have the option to save their breast by choosing breast conservation therapy. New treatment approaches have increased the choices available to women, in some cases eliminating the need for six weeks of traditional external beam radiation, and improving the patient’s quality of life.
The combination of lumpectomy and radiation therapy is commonly called breast-conserving therapy. Lumpectomy is the removal of the breast tumor (the "lump") and some of the normal tissue that surrounds it performed in a "breast conservation or preservation" manner.
Stereotactic Body Radiation Therapy for Lung Cancer is a highly focused form of radiation therapy that offers patients with early stage cancer a greater than 90% chance of success (local control) using a limited number of treatments (usually 5 days). For more advanced disease, a combination of radiation therapy, chemotherapy, and surgery may be utilized to optimize the chance of cure.
Stereotactic Body Radiation Therapy and Stereotactic Radio Surgery have great potential for improved outcomes as highlighted for Lung but must be executed with care and caution in a highly coordinated environment lead by board-certified radiation oncologists experienced with advanced treatment techniques.
Advanced Technology supporting the radiation team is the ELEKTA Infinity linear accelerator with the Agility 160 MLC. Florida Cancer Affiliates is the only oncology treatment center in the area utilizing 4D-CBCT guidance technology for daily Stereotactic Body Radiation Therapy/Stereotactic Radio Surgery treatment. This is critical technology when considering motion of lung tumors caused by breathing motion.
The ELEKTA Infinity supports External beam radiation therapy (EBRT) the most common form of radiotherapy using techniques such as 2D, 3D, IMRT (Intensity Modulated) or electrons to effectively treat a wide range of cancers such as Head and Neck, Breast Prostate, Lung and skin to name just a few. Stereotactic Radio Surgery is a unique form of EBRT that is precisely focused on a tumor within the brain that can be delivered a high dose in a single treatment while sparing normal brain tissue.
Stereotactic Body Radiation Therapy is a treatment procedure similar to Stereotactic Radio Surgery, except that it deals with tumors outside of the CNS such as Lung.
Florida Cancer Affiliates offers advanced radiation therapy technologies. These powerful, targeted, cancer-fighting treatments:
Radiation therapy may be delivered both externally and internally. Internal radiation, or brachytherapy, places a small amount of radioactive material (seeds) in or near the cancer. External radiation delivers high-energy rays directly at the cancer from a machine outside the body.
Bringing Each Patient the Best Care They Need Today
At Florida Cancer Affiliates, we are committed to providing patients with the best and most advanced, compassionate and comprehensive care available. We begin by offering the most current therapies proven to be effective, using the most advanced diagnostic and treatment technologies.
We continually evaluate the latest advances and proven treatments and identify a treatment plan that meets each patient’s individual needs. We consider many factors, including your medical history, current health, and risks and benefits of various treatment options.
When discussing your treatment options, we will tell you our goals and expected results for the treatment, as well as what can be expected during the treatment process. We find this type of clear communication is mutually beneficial and appreciated by our patients.
Bringing the Best in Care to You
At Florida Cancer Affiliates, we are committed to providing you with the best and most advanced, complete care available. We begin by offering therapies proven to be effective and advanced diagnostic and treatment technologies. We continue by providing unprecedented access to new investigational drugs through clinical trials.
To us, providing the best care means understanding that having cancer is difficult for patients and their families. Our physicians and staff are kind and compassionate, and will do whatever it takes to make everyone more at ease. From convenient parking to warm and friendly surroundings, our state-of-the-art centers are designed to make our patients comfortable. We believe care should be both advanced and compassionate.
We are leading the way to better care for patients with cancer or blood disorders by participating in many clinical trials that test new drugs, unique approaches to chemotherapy and radiation therapy, or various combinations of treatments. Not only does this push progress and advance cancer treatment, but it gives many of our patients the opportunity to receive promising new therapies and investigational drugs not yet available to patients outside these clinical trials.
Florida Cancer Affiliates is united in healing nationally with The US Oncology Network, one of the nation’s largest community-based cancer treatment and research networks. This means you have access to physicians who are connected nationwide, providing you with the most advanced therapies and treatment options, including unprecedented investigational drugs through clinical trials, close to home.
At Florida Cancer Affiliates, we provide the most advanced and personalized care to patients. Our team includes board certified Medical Oncology, Hematology, and Radiation Oncology physician specialists working together with oncology certified nurses, and certified radiation, imaging, laboratory and research professionals to provide patients with the best care in Bay, Citrus, Lake, Marion, and Sumter counties.
Florida Cancer Affiliates is united in healing with The US Oncology Network, one of the nation’s largest community-based cancer treatment and research networks focused on advancing cancer care in America. As an affiliate of The US Oncology Network, Florida Cancer Affiliates is united with more than 1,000 physicians and 10,000 cancer professionals nationwide.
The US Oncology Network is one of the largest community-based networks of doctors and practices in the country focused on cancer treatment and research. Each year, the more than 1,000 physicians in The Network touch the lives of more than 850,000 cancer patients in more than 540 locations and more than 80 integrated cancer centers throughout the United States.
Our pioneering, integrated approach to cancer care means that each patient’s cancer care team — medical oncologist, radiation oncologist and surgeon — collaborates to ensure delivery of the highest-quality and most advanced care to patients in the communities where they live.
US Oncology Research is the nation’s largest community-based research network specializing in Phase I through Phase IV oncology clinical trials. The investigator- and sponsor-initiated trials bring innovative therapies to patients in local communities across the nation. At any given time, we have more than 200 active clinical trials. We support 14 sites that offer Phase I trials, including first-in-human trials. Our research network has played a role in the development of 43 new cancer therapies approved by the FDA. To date, more than 49,000 patients have participated in our clinical trials, helping to advance the science of cancer care.
The US Oncology Network believes that all cancer patients should have access to the care they need without the threat of severe financial hardship. Patients are offered dedicated support to help access reimbursement- assistance programs. Since the program began in 2006, more than 25,000 patients from across the country received more than $150 million in financial assistance for needed therapies. We work with federal, state and local legislators, as well as government and private payers to foster a greater understanding about oncology patient care and the vital role community oncology practices play in the lives of cancer patients and their families.
The US Oncology Network’s pioneering, integrated approach to cancer care means that each patient’s cancer care team — medical oncologist, radiation oncologist and surgeon — collaborates to ensure delivery of the highest-quality and most advanced care to patients in the communities where they live.
Patients respond best to treatment when they receive integrated care close to home, relying on the support of family and friends and keeping their daily routines throughout the treatment process.
We are committed to giving patients access to the highest-quality, most advanced care close to home. Our 541 practice locations in The Network and more than 80 comprehensive cancer centers nationwide mean you can stay near your family and friends and keep your daily routine throughout your treatment process.
For more information, visit www.usoncology.com.
Staging is a careful attempt to find out the following:
When cancer of the pancreas spreads, the cancer cells may be found in nearby lymph nodes or the liver. Cancer cells may also be found in the lungs or in fluid collected from the abdomen.
When cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the original (primary) tumor. For example, if pancreatic cancer spreads to the liver, the cancer cells in the liver are actually pancreatic cancer cells. The disease is metastatic pancreatic cancer, not liver cancer. It’s treated as pancreatic cancer, not as liver cancer. Doctors sometimes call the new tumor in the liver “distant” disease.
To learn whether pancreatic cancer has spread, your doctor may order CT scans or EUS.
Also, a surgeon may look inside your abdomen with a laparoscope (a thin, tube-like device that has a light and a lens for seeing inside the body). The surgeon inserts the laparoscope through a small incision in your belly button. The surgeon will look for any signs of cancer inside your abdomen. You’ll need general anesthesia for this exam.
These are the stages of cancer of the pancreas:
Treatment options for people with cancer of the pancreas are surgery, chemotherapy, targeted therapy, and radiation therapy. You’ll probably receive more than one type of treatment.
The treatment that’s right for you depends mainly on the following:
At this time, cancer of the pancreas can be cured only when it’s found at an early stage (before it has spread) and only if surgery can completely remove the tumor. For people who can’t have surgery, other treatments may be able to help them live longer and feel better.
You may have a team of specialists to help plan your treatment. Specialists who treat cancer of the pancreas include surgeons, medical oncologists, radiation oncologists, and gastroenterologists.
Your health care team can describe your treatment choices, the expected results of each, and the possible side effects. Because cancer treatments often damage healthy cells and tissues, side effects are common. These side effects depend on many factors, including the type and extent of treatment. Side effects may not be the same for each person, and they may even change from one treatment session to the next. Before treatment starts, ask your health care team about possible side effects and how treatment may change your normal activities. You and your health care team can work together to develop a treatment plan that meets your needs.
Surgery may be an option for people with an early stage of pancreatic cancer. The surgeon usually removes only the part of the pancreas that has cancer. But, in some cases, the whole pancreas may be removed.
The type of surgery depends on the location of the tumor in the pancreas. Surgery to remove a tumor in the head of the pancreas is called a Whipple procedure. The Whipple procedure is the most common type of surgery for pancreatic cancer. You and your surgeon may talk about the types of surgery and which may be right for you.
In addition to part or all of your pancreas, the surgeon usually removes the following nearby tissues:
Also, the surgeon may remove your spleen and nearby lymph nodes.
Surgery for pancreatic cancer is a major operation. You will need to stay in the hospital for one to two weeks afterward. Your health care team will watch for signs of bleeding, infection, or other problems. It takes time to heal after surgery, and the time needed to recover is different for each person. You may have pain or discomfort for the first few days. It’s common to feel weak or tired for a while. You may need to rest at home for one to three months after leaving the hospital.
Chemotherapy uses drugs to kill cancer cells. Most people with pancreatic cancer get chemotherapy. For early pancreatic cancer, chemotherapy is usually given after surgery, but in some cases, it’s given before surgery. For advanced cancer, chemotherapy is used alone, with targeted therapy, or with radiation therapy.
Chemotherapy for pancreatic cancer is usually given by vein (intravenous). The drugs enter the bloodstream and travel throughout your body. Chemotherapy is given in cycles. Each treatment period is followed by a rest period. The length of the rest period and the number of cycles depend on the anticancer drugs used.
Some drugs used for pancreatic cancer also may cause tingling or numbness in your hands and feet.
People with cancer of the pancreas who can’t have surgery may receive a type of drug called targeted therapy along with chemotherapy.
Targeted therapy slows the growth of pancreatic cancer. It also helps prevent cancer cells from spreading. The drug is taken by mouth.
Side effects may include diarrhea, nausea, vomiting, a rash, and shortness of breath.
Radiation therapy uses high-energy rays to kill cancer cells. It can be given along with other treatments, including chemotherapy.
The radiation comes from a large machine. The machine aims beams of radiation at the cancer in the abdomen. You’ll go to a hospital or clinic 5 days a week for several weeks to receive radiation therapy. Each session takes about 30 minutes.
Although radiation therapy is painless, it may cause other side effects. The side effects include nausea, vomiting, or diarrhea. You may also feel very tired.
If you have symptoms that suggest cancer of the pancreas, your doctor will try to find out what’s causing the problems. You may have blood or other lab tests. Also, you may have one or more of the following tests:
Some doctors use the following tests also:
If cancer of the pancreas is diagnosed, your doctor needs to learn the extent (stage) of the disease to help you choose the best treatment.
There are two main types of pancreatic cancer.
Most often, pancreatic cancer starts in the ducts that carry pancreatic juices. This type is called exocrine pancreatic cancer. Information will focus on this type of pancreatic cancer.
Much less often, pancreatic cancer begins in the cells that make hormones. This type may be called endocrine pancreatic cancer or islet cell cancer.
Each year in the United States, more than 43,000 people are diagnosed with cancer of the pancreas. Most are over 65 years old. Visit the National Cancer Institute where this information and more can be found about Pancreatic Cancer or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el cáncer de páncreas en español.
People with early oral cancer may be treated with surgery or radiation therapy. People with advanced oral cancer may have a combination of treatments. For example, radiation therapy and chemotherapy are often given at the same time. Another treatment option is targeted therapy.
The choice of treatment depends mainly on your general health, where in your mouth or throat the cancer began, the size of the tumor, and whether the cancer has spread.
Surgery to remove the tumor in the mouth or throat is a common treatment for oral cancer. Sometimes the surgeon also removes lymph nodes in the neck. Other tissues in the mouth and neck may be removed as well. You may have surgery alone or in combination with radiation therapy.
Also, surgery may cause tissues in your face to swell. This swelling usually goes away within a few weeks. However, removing lymph nodes can result in swelling that lasts a long time.
Radiation therapy uses high-energy rays to kill cancer cells. It’s an option for small tumors or for people who can’t have surgery. Or, it may be used before surgery to shrink the tumor. It also may be used after surgery to destroy cancer cells that may remain in the area.
Doctors use two types of radiation therapy to treat oral cancer. Some people with oral cancer have both types:
Chemotherapy uses drugs to kill cancer cells. The drugs that treat oral cancer are usually given through a vein (intravenous). The drugs enter the bloodstream and travel throughout your body. Chemotherapy and radiation therapy are often given at the same time.
Some people with oral cancer receive a type of drug known as targeted therapy. It may be given along with radiation therapy or chemotherapy.
Cetuximab (Erbitux) was the first targeted therapy approved for oral cancer. Cetuximab binds to oral cancer cells and interferes with cancer cell growth and the spread of cancer. You may receive cetuximab through a vein once a week for several weeks at the clinic.
If oral cancer is diagnosed, your doctor needs to learn the extent (stage) of the disease to help you choose the best treatment. When oral cancer spreads, cancer cells may be found in the lymph nodes in the neck or in other tissues of the neck. Cancer cells can also spread to the lungs, liver, bones, and other parts of the body.
When cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells as the primary (original) tumor. For example, if oral cancer spreads to the lungs, the cancer cells in the lungs are actually oral cancer cells. The disease is called metastatic oral cancer, not lung cancer. It’s treated as oral cancer, not lung cancer. Doctors sometimes call the new tumor “distant” or metastatic disease.
Your doctor may order one or more of the following tests:
Doctors describe the stage of oral cancer based on the size of the tumor, whether it has invaded nearby tissues, and whether it has spread to the lymph nodes or other tissues:
If you have symptoms that suggest oral cancer, your doctor or dentist will check your mouth and throat for red or white patches, lumps, swelling, or other problems. A physical exam includes looking carefully at the roof of your mouth, back of your throat, and insides of your cheeks and lips. The floor of your mouth and lymph nodes in your neck will also be checked.
An ear, nose, and throat specialist can see the back of your nose, tongue, and throat by using a small, long-handled mirror or a lighted tube. Sometimes pictures need to be made with a CT scan or MRI to find a hidden tumor. (The Staging section describes imaging tests.)
The removal of a small piece of tissue to look for cancer cells is called a biopsy. Usually, a biopsy is done with local anesthesia. Sometimes, it’s done under general anesthesia. A pathologist then looks at the tissue under a microscope to check for cancer cells. A biopsy is the only sure way to know if the abnormal area is cancer.
Cancer that forms in tissues of the oral cavity (the mouth) or the oropharynx (the part of the throat at the back of the mouth).
This includes areas under the tongue
This includes areas of the throat
Visit the National Cancer Institute where this information and more can be found about Oral Cancer or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el cáncer oral en español.
Common treatment options for people with kidney cancer are surgery, targeted therapy, and biological therapy. You may receive more than one type of treatment.
The treatment that’s right for you depends mainly on the following:
Surgery is the most common treatment for people with kidney cancer. The type of surgery depends on the size and stage of the cancer, whether you have two kidneys, and whether cancer was found in both kidneys.
You and your surgeon can talk about the types of surgery and which may be right for you:
There are two approaches for removing the kidney. The surgeon may remove the tumor by making a large incision into your body (open surgery). Or the surgeon may remove the tumor by making small incisions (laparoscopic surgery). The surgeon sees inside your abdomen with a thin, lighted tube (a laparoscope) placed inside a small incision.
The surgeon may use other methods of destroying the cancer in the kidney. For people who have a tumor smaller than 4 centimeters and who can’t have surgery to remove part of the kidney because of other health problems, the surgeon may suggest:
People with kidney cancer that has spread may receive a type of drug called targeted therapy. Many kinds of targeted therapy are used for kidney cancer. This treatment may shrink a kidney tumor or slow its growth.Usually, the targeted therapy is taken by mouth. You may want to read the NCI fact sheet Targeted Cancer Therapies.
People with kidney cancer that has spread may receive biological therapy. Biological therapy for kidney cancer is a treatment that may improve the body’s natural defense (the immune system response) against cancer. The treatments used for kidney cancer can slow the growth of tumors or shrink them. The biological therapy is injected intravenously or under the skin. The treatment may be given at the hospital or a doctor’s office.
If kidney cancer is diagnosed, your doctor needs to learn the extent (stage) of the disease to help you choose the best treatment. The stage is based on the size of the kidney tumor and whether the cancer has invaded nearby tissues or spread to other parts of the body.
Your doctor may order one or more tests:
When cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary (original) tumor. For example, if kidney cancer spreads to a lung, the cancer cells in the lung are actually kidney cancer cells. The disease is metastatic kidney cancer, not lung cancer. It’s treated as kidney cancer, not as lung cancer.
These are the stages of kidney cancer:
If you have symptoms that suggest kidney cancer, your doctor will try to find out what’s causing the problems.
You may have a physical exam. Also, you may have one or more of the following tests:
Kidney cancer is a cancer that forms in tissues of the kidneys. Kidney cancer includes renal cell carcinoma (cancer that forms in the lining of very small tubes in the kidney that filter the blood and remove waste products) and renal pelvis carcinoma (cancer that forms in the center of the kidney where urine collects). It also includes Wilms tumor, which is a type of kidney cancer that usually develops in children under the age of 5.
Visit the National Cancer Institute where this information and more can be found about Kidney Cancer or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el cáncer de riñón en español.
Treatment options for people with uterine cancer are surgery, radiation therapy, chemotherapy, and hormone therapy. You may receive more than one type of treatment.
Surgery is the most common treatment for women with uterine cancer. You and your surgeon can talk about the types of surgery (hysterectomy) and which may be right for you.
The surgeon usually removes the uterus, cervix, and nearby tissues. The nearby tissues may include:
Surgery to remove lymph nodes may cause lymphedema (swelling) in one or both legs. Your health care team can tell you how to prevent or relieve lymphedema.
Radiation therapy is an option for women with all stages of uterine cancer. It may be used before or after surgery. For women who can’t have surgery for other medical reasons, radiation therapy may be used instead to destroy cancer cells in the uterus. Women with cancer that invades tissue beyond the uterus may have radiation therapy and chemotherapy.
Radiation therapy uses high-energy rays to kill cancer cells. It affects cells in the treated area only.
Doctors use two types of radiation therapy to treat uterine cancer. Some women receive both types:
Chemotherapy uses drugs to kill cancer cells. It may be used after surgery to treat uterine cancer that has an increased risk of returning after treatment. For example, uterine cancer that is a high grade or is Stage II, III, or IV may be more likely to return. Also, chemotherapy may be given to women whose uterine cancer can’t be completely removed by surgery. For advanced cancer, it may be used alone or with radiation therapy.
Chemotherapy for uterine cancer is usually given by vein (intravenous). It’s usually given in cycles. Each cycle has a treatment period followed by a rest period.
Some uterine tumors need hormones to grow. These tumors have hormone receptors for the hormones estrogen, progesterone, or both. If lab tests show that the tumor in your uterus has these receptors, then hormone therapy may be an option.
Hormone therapy may be used for women with advanced uterine cancer. Also, some women with Stage I uterine cancer who want to get pregnant and have children choose hormone therapy instead of surgery.The most common drug used for hormone therapy is progesterone tablets.
If you have symptoms that suggest uterine cancer, your doctor will try to find out what’s causing the problems. You may have a physical exam and blood tests. Also, you may have one or more of the following tests:
If cancer is found, the pathologist studies tissue samples from the uterus under a microscope to learn the grade of the tumor. The grade tells how much the tumor tissue differs from normal uterine tissue. It may suggest how fast the tumor is likely to grow. Tumors with higher grades tend to grow faster than those with lower grades. Tumors with higher grades are also more likely to spread. Doctors use tumor grade along with other factors to suggest treatment options.
If uterine cancer is diagnosed, your doctor needs to learn the extent (stage) of the disease to help you choose the best treatment. The stage is based on whether the cancer has invaded nearby tissues or spread to other parts of the body.
When cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary (original) tumor. For example, if uterine cancer spreads to the lung, the cancer cells in the lung are actually uterine cancer cells. The disease is metastatic uterine cancer, not lung cancer. It’s treated as uterine cancer, not as lung cancer. Doctors sometimes call the new tumor “distant” disease.
To learn whether uterine cancer has spread, your doctor may order one or more tests:
In most cases, surgery is needed to learn the stage of uterine cancer. The surgeon removes the uterus and may take tissue samples from the pelvis and abdomen. After the uterus is removed, it is checked to see how deeply the tumor has grown. Also, the other tissue samples are checked for cancer cells.
These are the stages of uterine cancer:
Endometrial cancer is a cancer that forms in the tissue lining the uterus (the small, hollow, pear-shaped organ in a woman’s pelvis in which a fetus develops). Most endometrial cancers are adenocarcinomas (cancers that begin in cells that make and release mucus and other fluids).
Visit the National Cancer Institute where this information and more can be found about Endometrial Cancer including side effects of treatments, support information and more. Or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el cáncer de endometrio en español.
Cigarette Smoking and Tobacco Use
Tobacco use is strongly linked to an increased risk for many kinds of cancer. Smoking cigarettes is the leading cause of the following types of cancer:
Not smoking or quitting smoking lowers the risk of getting cancer and dying from cancer. Scientists believe that cigarette smoking causes about 30% of all cancer deaths in the United States.
See the following National Cancer Institute PDQ summaries for more information:
Infections
Certain viruses and bacteria may be able to cause cancer. Viruses and other infection-causing agents cause more cases of cancer in the developing world (about 1 in 4 cases of cancer) than in developed nations (less than 1 in 10 cases of cancer). Examples of cancer-causing viruses and bacteria include:
Two vaccines prevent infection by cancer-causing agents have already been developed and approved by the U.S. Food and Drug Administration (FDA). One is a vaccine to prevent infection with hepatitis B virus. The other protects against infection with strains of human papillomavirus (HPV) that cause cervical cancer. Scientists continue to work on vaccines against infections that cause cancer.
See the following National Cancer Institute PDQ summaries for more information:
Radiation
Being exposed to radiation is a known cause of cancer. There are two main types of radiation linked with an increased risk for cancer:
See the following National Cancer Institute PDQ summaries for more information:
Diet
The foods that you eat on a regular basis make up your diet. Diet is being studied as a risk factor for cancer. It is hard to study the effects of diet on cancer because a person’s diet includes foods that may protect against cancer and foods that may increase the risk of cancer.
It is also hard for people who take part in the studies to keep track of what they eat over a long period of time. This may explain why studies have different results about how diet affects the risk of cancer.
Some studies show that fruits and nonstarchy vegetables may protect against cancers of the mouth, esophagus, and stomach. Fruits may also protect against lung cancer.
Some studies have shown that a diet high in fat, proteins, calories, and red meat increases the risk of colorectal cancer, but other studies have not shown this.
It is not known if a diet low in fat and high in fiber, fruits, and vegetables lowers the risk of colorectal cancer. See the American Institute for Cancer Research for more information about foods that prevent cancer.
See the following PDQ summaries for more information:
Alcohol
Studies have shown that drinking alcohol is linked to an increased risk of the following types of cancers:
Drinking alcohol may also increase the risk of liver cancer and female colorectal cancer.
See the following National Cancer Institute PDQ summaries for more information:
Physical Activity
Studies show that people who are physically active have a lower risk of certain cancers than those who are not. It is not known if physical activity itself is the reason for this.
Studies show a strong link between physical activity and a lower risk of colorectal cancer. Some studies show that physical activity protects against postmenopausal breast cancer and endometrial cancer.
See the following National Cancer Institute PDQ summaries for more information:
Obesity
Studies show that obesity is linked to a higher risk of the following types of cancer:
Some studies show that obesity is also a risk factor for cancer of the gallbladder.
Studies do not show that losing weight lowers the risk of cancers that have been linked to obesity.
See the following National Cancer Institute PDQ summaries for more information:
Information provided the National Cancer Institute.
Although there are many kinds of cancer, they all start because of out-of-control growth of abnormal cells. Normal body cells grow, divide, and die in an orderly fashion. Because cancer cells continue to grow and divide, they are different from normal cells. Instead of dying, they outlive normal cells and continue to form new abnormal cells.
When this abnormal cell growth occurs, the result can be the development of a lump, mass or tumor, which can be benign (non-cancerous) or malignant (cancerous). Cancer cells develop because of damage to DNA, which directs all activities in each cell. When DNA becomes damaged, the body is usually able to repair it. In cancer cells, however, the damaged DNA is not repaired.
Cancer comes in many forms, and the specific disease is named for the part of the body in which it begins. Cells from cancerous tumors can spread, or metastasize, throughout the body. For example, cancer that begins in the prostate but has spread to the bones is called metastatic prostate cancer. Some cancers involving the blood and blood-forming organs (bone marrow) do not form tumors, but circulate through other tissues where they grow.
Today, millions of people are living with cancer or have had cancer. Florida Cancer Affiliates offers this extensive disease and drug information section with the intent of helping you learn more about cancer, and what you can expect for the "typical treatment" of common types of cancer.
Use this information to help you better understand the disease and make informed and timely choices for your treatment. Then speak with your Florida Cancer Affiliate physician about how a customized treatment plan will be developed to meet your specific care needs.
Our expert physicians and clinical staff are ready to help you, your family and caretakers through every step of this cancer journey.
Appointments
We know that patients facing cancer need rapid answers and the best treatment plans. To schedule your appointment, please call (352) 732-4032 and ask for the location that is nearest you.
Questions
For questions or inquiries related to your physician, appointments, prescriptions, PET scans, lab work, or to speak to your nurse, please call the specific physician office that you visit. .
Employment
Please fax resumes and employment inquiries to the HR Coordinators at 727.484.7782.
Florida Cancer Affiliates is a practice in The US Oncology Network (The Network). This collaboration unites the practice with more than 1,200 independent physicians dedicated to delivering value-based, integrated care to patients — close to home. Through The Network, these independent doctors come together to form a community of shared expertise and resources dedicated to advancing local cancer care and to delivering better patient outcomes. The Network is supported by McKesson Corporation, whose coordinated resources and infrastructure allow doctors in The Network to focus on the health of their patients, while McKesson focuses on the health of their practices. Florida Cancer Affiliates also participates in clinical trials through US Oncology Research, which has played a role in more than 100 FDA-approved cancer therapies, approximately one-third of all cancer therapies approved by the FDA to date. For more information, visit usoncology.com
New Port Richey
5500 Little Road
New Port Richey, FL
34655
Tel 727.372.9159
Fax 727.376.8703
Spring Hill
11373 Cortez Boulevard # Suite 200
Brooksville, FL
34613
Tel 352.597.4998
Fax 352.596.6051
Patients who fill out their patient forms, prior to their initial visit are more at ease during their appointment. It also saves you valuable time while you’re in our office.
To fill out your New Patient forms, click on the link below, print the form, and fill out as many fields as possible. Bring the forms with you to your first visit. Please take your time when filling out the forms, and provide as much information as you can about your complete health history.
Click here for the FCA Patient History Form.
Click here for the FCA HIPAA From.
Click here for the FCA Assignment of Benefits form.
While a person experiences a variety of emotions, when a person first learns that he/she has cancer or a blood disorder/disease, the primary concern is survival. As treatment begins, however, new issues become important. Some of these include relationships with others, side effects from treatments, and nutrition and diet. Living with cancer or a blood disease/disorder is challenging, and it is best to be educated about issues surrounding survival in order to live a full and productive life.
Below are links to websites containing information for people living with cancer or a blood disorder/disease. The content provided through these links is not the information of Cancer Care Centers of South Texas nor does the practice necessarily endorse such content. In addition, all content provided through these links is for information only and does not constitute medical advice. Please consult your physician before acting or relying upon such information.
American Cancer Society (ACS)
English
Espanol
American College of Radiation Oncology (ACRO)
www.acro.org
American Institute of Cancer Resarch
American Medical Association (AMA)
www.ama-assn.org
American Society of Hematology (ASH)
www.hematology.org
American Society for Therapeutic Radiology and Oncology (ASTRO)
www.astro.org
American Society of Clinical Oncology (ASCO)
www.asco.org
Association of Cancer Online Resources (ACOR)
www.acor.org
CancerEducation.com
www.cancereducation.com
Cancer News on the Net®
www.cancernews.com
Cancer Research Institute (CRI)
www.cancerresearch.org
Cancer.net
www.cancer.net
CancerGuide
www.cancerguide.org
Healthfinder
www.healthfinder.gov
Medline Plus
www.nlm.nih.gov/medlineplus
Myelodysplastic Syndromes Foundation
National Alliance for Caregiving (NAC)
www.caring.org
National Cancer Institute (NCI)
English
Espanol
National Comprehensive Cancer Network (NCCN)
www.nccn.org
Needy Meds
www.needymeds.com
National Institutes of Health (NIH)
www.nih.gov
National Library of Medicine (NLM)
www.nlm.nih.gov
OncoLink (University of Pennsylvania)
www.oncolink.org
Oncology Nursing Society (ONS)
www.ons.org
Planet Cancer
www.planetcancer.org
Quackwatch
www.quackwatch.com
Society of Gynecologic Oncologists
www.sgo.org
U.S. Food and Drug Administration (FDA)
www.fda.gov
US Oncology
www.usoncology.com
National Brain Tumor Society
www.braintumor.org
BreastCancer.org
www.breastcancer.org
Breast Cancer Network of Strength
(formerly Y-ME National Breast Cancer Organization)
www.networkofstrength.org
Colon Cancer Alliance
www.ccalliance.org
Leukemia & Lymphoma Society
www.leukemia-lymphoma.org
Lung Cancer Alliance
www.lungcanceralliance.org
Lymphoma Research Foundation
www.lymphoma.org
Ovarian Cancer National Alliance
www.ovariancancer.org
National Ovarian Cancer Coalition
www.ovarian.org
Prostate Cancer Foundation
www.pcf.org
Skin Cancer Foundation
www.skincancer.org
Alamo Breast Cancer Foundation
www.alamobreastcancer.org
Alamo City Cancer Council
www.alamocitycancercouncil.org
Leukemia/Lymphoma Society South Texas Chapter
www.leukemia-lymphoma.org/all_chap
Susan G. Komen San Antonio Chapter
www.komensanantonio.org
National Coalition for Cancer Survivorship
www.canceradvocacy.org
Cancer Survivors Network
csn.cancer.org
National Cancer Survivor Day® Foundation, Inc.
www.ncsdf.org
National Patient Advocate Foundation (NPAF)
www.npaf.org
Patient Advocate Foundation
www.patientadvocate.org
Caring Connections
www.caringinfo.org
Gilda’s Club Worldwide
www.gildasclub.org
Lance Armstrong Foundation
www.livestrong.org
Life Beyond Cancer Foundation
www.lifebeyondcancer.org
Look Good…Feel Better
English
Espanol
National Center for Complementary and Alternative Medicine
www.nccam.nih.gov
National Family Caregivers Association (NFCA)
www.nfcacares.org
People Living Through Cancer
www.pltc.org
US TOO Prostate Cancer Support Group
www.ustoo.com
The Wellness Community
www.thewellnesscommunity.org
People with multiple myeloma have many treatment options. The options are watchful waiting, induction therapy, and stem cell transplant. Sometimes a combination of methods is used.
Radiation therapy is used sometimes to treat painful bone disease. It may be used alone or along with other therapies. See the Supportive Care section to learn about ways to relieve pain.
The choice of treatment depends mainly on how advanced the disease is and whether you have symptoms. If you have multiple myeloma without symptoms (smoldering myeloma), you may not need cancer treatment right away. The doctor monitors your health closely (watchful waiting) so that treatment can start when you begin to have symptoms.
If you have symptoms, you will likely get induction therapy. Sometimes a stem cell transplant is part of the treatment plan.
When treatment for myeloma is needed, it can often control the disease and its symptoms. People may receive therapy to help keep the cancer in remission, but myeloma can seldom be cured. Because standard treatment may not control myeloma, you may want to talk to your doctor about taking part in a clinical trial. Clinical trials are research studies of new treatment methods.
People with smoldering myeloma or Stage I myeloma may be able to put off having cancer treatment. By delaying treatment, you can avoid the side effects of treatment until you have symptoms.
If you and your doctor agree that watchful waiting is a good idea, you will have regular checkups (such as every 3 months). You will receive treatment if symptoms occur.
Although watchful waiting avoids or delays the side effects of cancer treatment, this choice has risks. In some cases, it may reduce the chance to control myeloma before it gets worse.
You may decide against watchful waiting if you don’t want to live with untreated myeloma. If you choose watchful waiting but grow concerned later, you should discuss your feelings with your doctor. Another approach is an option in most cases.
Many different types of drugs are used to treat myeloma. People often receive a combination of drugs, and many different combinations are used to treat myeloma.
Each type of drug kills cancer cells in a different way:
You may receive the drugs by mouth or through a vein (IV). The treatment usually takes place in an outpatient part of the hospital, at your doctor’s office, or at home. Some people may need to stay in the hospital for treatment.
Many people with multiple myeloma may get a stem cell transplant. A stem cell transplant allows you to be treated with high doses of drugs. The high doses destroy both myeloma cells and normal blood cells in the bone marrow. After you receive high-dose treatment, you receive healthy stem cells through a vein. (It’s like getting a blood transfusion.) New blood cells develop from the transplanted stem cells. The new blood cells replace the ones that were destroyed by treatment.
Stem cell transplants take place in the hospital. Some people with myeloma have two or more transplants.
Stem cells may come from you or from someone who donates their stem cells to you:
There are two ways to get stem cells for people with myeloma. They usually come from the blood (peripheral blood stem cell transplant). Or they can come from the bone marrow (bone marrow transplant).
After a stem cell transplant, you may stay in the hospital for several weeks or months. You’ll be at risk for infections because of the large doses of chemotherapy you received. In time, the transplanted stem cells will begin to produce healthy blood cells.
If the biopsy shows that you have multiple myeloma, your doctor needs to learn the extent (stage) of the disease to plan the best treatment. Staging may involve having more tests:
Doctors may describe multiple myeloma as
The stage takes into account whether the cancer is causing problems with your bones or kidneys. Smoldering multiple myeloma is early disease without any symptoms. For example, there is no bone damage. Early disease with symptoms (such as bone damage) is Stage I. Stage II or III is more advanced, and more myeloma cells are found in the body.
Doctors sometimes find multiple myeloma after a routine blood test. More often, doctors suspect multiple myeloma after an x-ray for a broken bone. Usually though, patients go to the doctor because they are having other symptoms.
To find out whether such problems are from multiple myeloma or some other condition, your doctor may ask about your personal and family medical history and do a physical exam. Your doctor also may order some of the following tests:
There are two ways your doctor can obtain bone marrow. Some people will have both procedures during the same visit:
Myeloma begins when a plasma cell becomes abnormal. The abnormal cell divides to make copies of itself. The new cells divide again and again, making more and more abnormal cells. These abnormal plasma cells are called myeloma cells.
In time, myeloma cells collect in the bone marrow. They may damage the solid part of the bone. When myeloma cells collect in several of your bones, the disease is called “multiple myeloma.” This disease may also harm other tissues and organs, such as the kidneys.
Myeloma cells make antibodies called M proteins and other proteins. These proteins can collect in the blood, urine, and organs.
Visit the National Cancer Institute where this information and more can be found about Multiple Myeloma or ask your cancer care team questions about your individual situation.
Your doctor can describe your treatment choices and the expected results. You and your doctor can work together to develop a treatment plan that meets your needs.
Your doctor may refer you to a specialist, or you may ask for a referral. Specialists who treat Hodgkin lymphoma include hematologists, medical oncologists, and radiation oncologists . Your doctor may suggest that you choose an oncologist who specializes in the treatment of Hodgkin lymphoma. Often, such doctors are associated with major academic centers. Your health care team may also include an oncology nurse and a registered dietitian.
The choice of treatment depends mainly on the following:
People with Hodgkin lymphoma may be treated with chemotherapy, radiation therapy, or both.
If Hodgkin lymphoma comes back after treatment, doctors call this a relapse or recurrence. People with Hodgkin lymphoma that comes back after treatment may receive high doses of chemotherapy, radiation therapy, or both, followed by stem cell transplantation.
Chemotherapy for Hodgkin lymphoma uses drugs to kill lymphoma cells. It is called systemic therapy because the drugs travel through the bloodstream. The drugs can reach lymphoma cells in almost all parts of the body.
Usually, more than one drug is given. Most drugs for Hodgkin lymphoma are given through a vein (intravenous), but some are taken by mouth.
Chemotherapy is given in cycles. You have a treatment period followed by a rest period. The length of the rest period and the number of treatment cycles depend on the stage of your disease and on the anticancer drugs used.
You may have your treatment in a clinic, at the doctor’s office, or at home. Some people may need to stay in the hospital for treatment.
Radiation therapy (also called radiotherapy) for Hodgkin lymphoma uses high-energy rays to kill lymphoma cells. It can shrink tumors and help control pain.
A large machine aims the rays at the lymph node areas affected by lymphoma. This is local therapy because it affects cells in the treated area only. Most people go to a hospital or clinic for treatment 5 days a week for several weeks.
If Hodgkin lymphoma returns after treatment, you may receive stem cell transplantation. A transplant of your own blood-forming stem cells (autologous stem cell transplantation) allows you to receive high doses of chemotherapy, radiation therapy, or both. The high doses destroy both Hodgkin lymphoma cells and healthy blood cells in the bone marrow.
Stem cell transplants take place in the hospital. Before you receive high-dose treatment, your stem cells are removed and may be treated to kill lymphoma cells that may be present. Your stem cells are frozen and stored. After you receive high-dose treatment to kill Hodgkin lymphoma cells, your stored stem cells are thawed and given back to you through a flexible tube placed in a large vein in your neck or chest area. New blood cells develop from the transplanted stem cells.
The doctor considers the following to determine the stage of Hodgkin lymphoma:
The stages of Hodgkin lymphoma are as follows:
In addition to these stage numbers, your doctor may also describe the stage as A or B:
If you have swollen lymph nodes or another symptom that suggests Hodgkin lymphoma, your doctor will try to find out what’s causing the problem. Your doctor may ask about your personal and family medical history.
You may have some of the following exams and tests:
The pathologist uses a microscope to check the tissue for Hodgkin lymphoma cells. A person with Hodgkin lymphoma usually has large, abnormal cells known as Reed-Sternberg cells. They are not found in people with non-Hodgkin lymphoma. See the photo of a Reed-Sternberg cell.
Hodgkin lymphoma is a cancer that begins in cells of the immune system. The immune system fights infections and other diseases.
Hodgkin lymphoma can start almost anywhere. Usually, it's first found in a lymph node above the diaphragm, the thin muscle that separates the chest from the abdomen. But Hodgkin lymphoma also may be found in a group of lymph nodes. Sometimes it starts in other parts of the lymphatic system.
Hodgkin Lymphoma Cells
Hodgkin lymphoma begins when a lymphocyte (usually a B cell) becomes abnormal. The abnormal cell is called a Reed-Sternberg cell. (See photo below.)
The Reed-Sternberg cell divides to make copies of itself. The new cells divide again and again, making more and more abnormal cells. The abnormal cells don't die when they should. They don't protect the body from infections or other diseases. The buildup of extra cells often forms a mass of tissue called a growth or tumor.
Visit the National Cancer Institute where this information and more can be found about Hodgkin Lymphoma or ask your cancer care team questions about your individual situation.
Lo que usted necesita saber sobre el linfoma de Hodgkin.
Read the Press Release
FCA physicians first in the state of Florida certified to safely administer the SpaceOAR hydrogel technology for prostate cancer patients receiving radiation therapy.
At FCA, we are dedicated to finding new and better ways to treat cancer through research and clinical trials. We have access to clinical trials through our partnership with The US Oncology Network, one of the nation's largest community-based cancer treatment and research networks. Click to View Available Trials